Classification of lesions has very relevant consequences, not only in terms of patient outcome but also for further diagnostic assessment in the context of increasing expenditure incurred by health systems. For breast lesions, BI-RADS 3 allows the possibility of a "wait and see" approach instead of immediate biopsy. Given the growing number of incidental benign findings during screening and clinical breast imaging, this can be a key benefit.
The BI-RADS descriptors and classification system has provided a common formal language. Before it was established, confusing terms such as fibrocystic disease or dysplasia were commonly used in reports, and many general physicians would mistakenly think a patient had a premalignant disease when the report simply described normal breasts displaying high density patterns.
Another advantage of BI-RADS has been the introduction in the radiology report of a recommendation, including follow-up imaging and interventional procedures. This increases the radiologist's responsibility and also enhances his or her clinical role. But a limitation of the system pertains predominantly to the BI-RADS 3 category, which relates to cases of less than 2% probability of cancer, a rate which can only be evaluated retrospectively on a large number of cases.
"The classification system isn't an exact science. The main potential pitfall is incorrect classification," said Dr. Luis J. Pina, a radiologist at the University Clinic of Navarra in Spain and a speaker at Friday's special focus session. "Specifically, the BI-RADS 3 category can become a 'holding tank' for problematic lesions which are so categorized without further diagnostic procedures. This typically occurs when inexperienced radiologists feel uncertain about diagnosis."
If a BI-RADS 4 or 5 lesion is erroneously classified as category 3, the diagnosis of malignancy will be delayed. Conversely, if a BI-RADS 2 lesion is classified as category 3, patients may undergo unnecessary anxiety and potentially needless intervention.
Incorrect classification may not be just a question of inexperience. Differences in how BI-RADS is adopted as a common language also may lead to problems of classification, according to Dr. Francesco Sardanelli, EuroAIM director at the University of Milan School of Medicine and head of radiology at the IRCCS Policlinico San Donato, Milan.
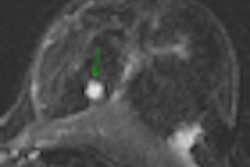
"How many radiologists specifically know that you can give a BI-RADS score to a lesion, to a breast, to a woman, for a single examination or for the series of examinations?" asked Sardanelli. "After a breast MRI is performed as a third step after mammography and ultrasound, a conclusive BI-RADS must be defined at the end of the report; a suspicious cluster of microcalcifications, even though nonenhancing on MRI, remains a BI-RADS 4 because it may be a ductal carcinoma in situ (DCIS) with low angiogenesis."
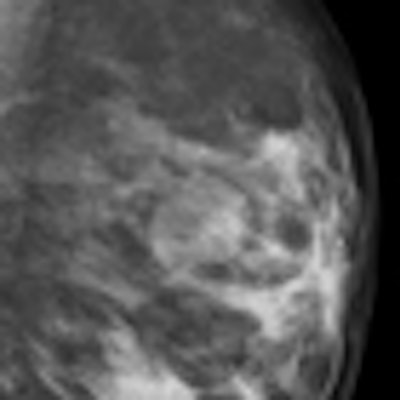
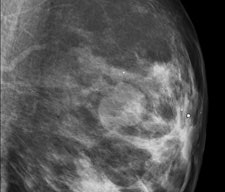
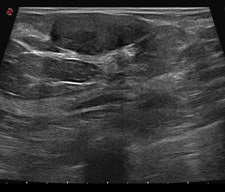
After detection of a possible lesion using a front-line method such as standard two-view mammography, additional techniques should be used if there is reasonable suspicion of cancer. Superimposed breast tissue can mimic a malignant lesion. If the lesion exists, other techniques can help the radiologist to decide about the degree of concern and to classify the lesion correctly. These were discussed during Friday's session. In addition, speakers covered the influence of clinical data on classification.
Risk profile is increasingly important in personalized medicine, and this is equally true in breast imaging. Carriers of BRCA1 or BRCA2, high risk related to a previous cancer, and a high-risk lesion such as lobular neoplasia, atypical ductal hyperplasia, or papillomatosis all change the likelihood of cancer for a "probably benign" finding initially thought to be BI-RADS 3 to BI-RADS 4. Management must then be changed accordingly.
"Positive family history for breast cancer, the presence of a lump or a palpable lesion, nipple discharge, pregnancy or the intention to become pregnant, a recently diagnosed breast cancer, and many other circumstances influence the final assessment," Pina said.
In screening, BI-RADS 3 should be avoided, particularly because some screening program do not allow for a three to six month re-evaluation. In the clinical setting, the low positive predictive value (PPV) of BI-RADS 3 makes a short interval follow-up possible as an alternative to biopsy.
Today most biopsies are performed percutaneously in an outpatient setting, under local anesthesia, with no scarring and at low cost. This evolution in breast biopsy has resulted in increasing numbers of biopsies, even in probably benign lesions.
Experts point to the fact that the definition of less than 2% probability of cancer is often ignored. A relatively large number of BI-RADS 3 findings tend to be biopsied due to the category being confused with R3, the European category of findings with a relatively low cancer probability but with a probability that is still higher than BI-RADS 3.
"Prospectively speaking, radiologists should put all the cases they believe to be associated with a cancer probability from 2% to 95% in the category of BI-RADS 4," Sardanelli said.
In an ideal world there would be no BI-RADS 3 classifications, according to Pina. Recognizing the impossibility of this, however, he suggests that this controversial classification should not exceed 7% of all mammograms.
"Even this figure can be reduced through previous imaging comparison and complementary studies, including nonimaging findings such as palpation, clinical symptoms, and history," he noted.
Delegates at Friday's session were likely seeking clear "golden" management rules on when to biopsy a BI-RADS 3 lesion and when to watch, particularly if they are keen to understand how to reduce the risk of legal consequences of delaying cancer diagnosis because of using this category. For Sardanelli, the answer is clear: Cases of a PPV for cancer of less than 2% should be checked and checked again.
"Radiologists should be trained for the responsibility of diagnosis. This is what they are paid for," he stressed. "If, and only if, your BI-RADS 3 categorization is correct, then unless the patient is anxious about waiting, the logical choice is to watch and follow up at six months. The only alternative is to perform a large number of useless biopsies that would reduce your credibility and that of the center where you work."
Originally published in ECR Today March 4, 2011.
Copyright © 2011 European Society of Radiology