MRI can be of value for detecting cancer recurrence in the treated breast, but it continues to arouse controversy when it comes to other indications. Any discussion of the potential applications of MRI for pretreatment and for screening high-risk populations tends to raise more questions than answers.
There is an urgent need for radiologists to be clear about the indications for MRI and to be aware of its advantages and limitations, especially in cases of high risk, noted Dr. Corinne Balleyguier, a radiological cancer specialist at Institut Gustave Roussy, Villejuif, Paris. Women carrying the BRCA1 or BRCA2 genes have a 70% to 80% chance of developing cancer, and require a yearly examination with mammography, ultrasound, and MRI, and while ultrasound and mammography can detect around half of cancers in younger women with denser breasts in this population, MRI can detect between 80% and 100%, she added.
"One of the main problems with breast MRI is that its high sensitivity makes for a 'false positive' rate of 20% to 30% in this indication, with the potential of some of these false positives resulting in stressful and expensive MR-guided biopsies. Despite this, the advantages of MRI for these high-risk patients outweigh the danger of false positives," said Balleyguier, a speaker at Friday's refresher course on breast MRI.
A gain in survival for BRCA1 mutation carriers due to an earlier diagnosis of highly aggressive triple-negative cancers with MRI is probable, but still has to be demonstrated.
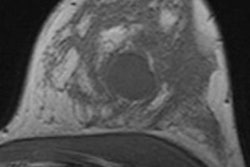
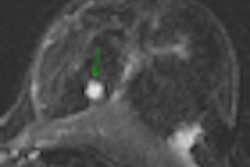
 Breast cancer staging in a 42-year-old woman using sagittal 3D sequence with gadolinium chelates injection, subtraction. A bifocal lesion is seen on this view. The size of the largest lesion was 50 mm. Mammography and ultrasound only depicted a unique 40-mm lesion. Breast MRI can be a valuable imaging tool for staging lobular infiltrative carcinoma, as in this case. Image courtesy of Dr. Corinne Balleyguier.
Breast cancer staging in a 42-year-old woman using sagittal 3D sequence with gadolinium chelates injection, subtraction. A bifocal lesion is seen on this view. The size of the largest lesion was 50 mm. Mammography and ultrasound only depicted a unique 40-mm lesion. Breast MRI can be a valuable imaging tool for staging lobular infiltrative carcinoma, as in this case. Image courtesy of Dr. Corinne Balleyguier.
"Another issue still open to debate is the possibility that MRI in this indication can replace mammography, avoiding radiation exposure for high-risk patients. BRCA1 and BRCA2 mutation carriers who are more sensitive to radiation than the general population," said co-speaker Dr. Francesco Sardanelli, EuroAIM director, University of Milan School of Medicine and director of radiology at the IRCCS Policlinico San Donato, Italy, who focused on evidence-based controversies at Friday's session. Evidence-based medicine (EBM) is a key topic for medical professionalism, including that of radiologists, the goal of which concerns ethics (i.e., doing the best for patients) and economics (notably avoiding needless examinations and treatments), he elaborated.
Perhaps the most controversial indication of breast MRI to date is for staging of breast cancer. The discovery of additional cancers by MRI that were undetected by mammography during staging throws patient management into question, and so far no studies point to a clear gold standard, commented Sardanelli. "We see more with preoperative MRI but we do not know if this has a positive impact in terms of patient outcome. This debate will continue in the next few years and its conclusion is not around the corner."
Additional MRI findings have an impact on ipsilateral treatment planning in about 11% of patients, causing wider local excision or shifting from breast-conserving surgery to mastectomy, while in about 3% to 4% of patients, occult contralateral cancers are detected with MRI. "A percentage of these lesions -- how many, we do not know -- could be cured with radiation therapy or chemotherapy. Thus, there exists a real risk of overdiagnosis and overtreatment, especially for ipsilateral findings," he said.
Balleyguier echoed Sardanelli and pointed to the need for long-term studies of at least 10 years to follow patient outcomes.
"Although we know through a recent five-year study that recurrence is lower in patients who undergo pretreatment MRI, we don't know if these women survive longer than women who don't," said Balleyguier. "However, we know that recurrence rate is an element of poor proper prognosis. If we can avoid local recurrence and provide better treatment at the start, then it makes sense that survival will improve."
At Friday's session, she also discussed technical aspects for obtaining high-quality images, one among several criteria for optimal interpretation. Part of her talk dealt not only with the use of contrast but also the importance of T2 imaging to distinguish between malignant and benign lesions. "Benign and malignant lesions can both enhance. In this case, we look at T2-weighted imaging, and if the enhanced lesion is very bright, it is usually not a cancer but a benign lesion such as a lymph node or cellular fibroadenoma. Comparison of T2 and T1 plus contrast can help to decrease false positives."
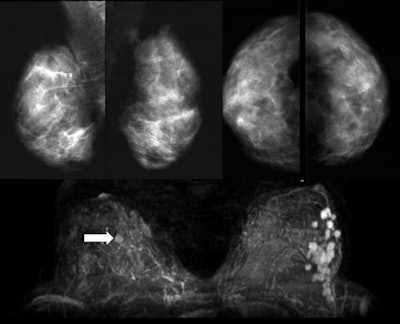 A 36-year-old woman with palpable nodules at the lower external left quadrant. Mammography (upper panels) shows an extremely dense pattern without any suspicious finding on either right or left breast. Ultrasound (not shown) demonstrated three hypoechoic nodules. One of them was biopsied, revealing invasive ductal cancer. MRI (lower panel) showed 22 suspicious enhancing lesions confined in the lower external quadrant of the left breast. Moreover, one enhancing lesion is found in the right breast (arrow), undetectable at targeted second-look ultrasound. The patient refused MR-guided biopsy of the contralateral lesion. Left mastectomy was performed, confirming multifocal cancer on the left. At one-year MRI follow-up after chemotherapy, the contralateral lesion was no longer detectable. Images courtesy of Dr. Francesco Sardanelli.
A 36-year-old woman with palpable nodules at the lower external left quadrant. Mammography (upper panels) shows an extremely dense pattern without any suspicious finding on either right or left breast. Ultrasound (not shown) demonstrated three hypoechoic nodules. One of them was biopsied, revealing invasive ductal cancer. MRI (lower panel) showed 22 suspicious enhancing lesions confined in the lower external quadrant of the left breast. Moreover, one enhancing lesion is found in the right breast (arrow), undetectable at targeted second-look ultrasound. The patient refused MR-guided biopsy of the contralateral lesion. Left mastectomy was performed, confirming multifocal cancer on the left. At one-year MRI follow-up after chemotherapy, the contralateral lesion was no longer detectable. Images courtesy of Dr. Francesco Sardanelli.The emerging role of diffusion-weighted imaging (DWI) in diagnosis also may promote discussion. Sardanelli identified new noncontrast MRI approaches such as highly spatially resolved water-selective sequences as the next decade's major trend. Refinement of current noncontrast approaches, especially DWI, may become a substitute for contrast-enhanced MRI, as has been demonstrated in studies on the detection of residual tumour after chemotherapy. This has potential implications for screening and for the general female population, but radiologists have to prove the high negative predictive value of these approaches in screening.
Balleyguier pointed to the possibility of clinical 3-tesla imaging with spectroscopy and DWI to detect more lesions and better characterize them, but she admitted that as yet there was not enough data to firmly support this development. The advantages and limitations of 3-tesla breast imaging also were discussed at the session. The role of CAD, in terms of kinetic tasks, lesion targeting for MR-guided biopsy, and correcting movement artifacts, as well as future developments in the pipeline for CAD morphology tasks, also was covered.
To improve image interpretation in breast MR, she thinks personal evaluation and auditing can be useful. Radiologists need to work on sequences with various protocols on different machines to improve quality, and results should be evaluated. If the radiologist detects additional lesions and the patient has to have surgery, then you should be interested in histological results and treatment to determine if the correct recommendations were made, she explained. "Radiologists must face the consequences of what they say to improve their level."
Originally published in ECR Today March 4, 2011.
Copyright © 2011 European Society of Radiology