Imaging plays a central role in evaluating and tracking kidney complications due to COVID-19 -- and radiologists must not only understand what to look for but also make themselves readily available to their referring colleagues, Italian experts told ECR 2021 attendees.
Imaging features of renal complications due to COVID-19 include renal parenchyma attenuation, perinephric fat stranding, and renal infarction (which can lead to vascular coagulopathy), presenter Prof. Riccardo Manfredi of the Gemelli University Hospital in Rome told session attendees. Manfredi also listed possible renal sequelae due to COVID-19, such as electrolyte dysfunction, acute kidney injury, and renal replacement therapy.
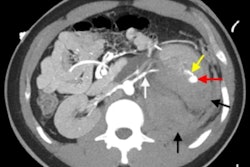
 Contrast-enhanced CT shows renal vascular injury in a patient with COVID-19. Findings include severe hypercoagulability state, renal infarction, and wedge-shaped hypoenhancing and nonenhancing areas. All images courtesy of Prof. Riccardo Manfredi.
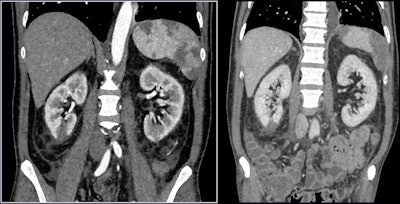
Contrast-enhanced CT shows renal vascular injury in a patient with COVID-19. Findings include severe hypercoagulability state, renal infarction, and wedge-shaped hypoenhancing and nonenhancing areas. All images courtesy of Prof. Riccardo Manfredi.The take-home message? Renal sequelae caused by COVID-19 disease are quite common, he said.
"Although imaging findings [of renal complications due to COVID-19] may not be specific, renal parenchyma attenuation and perinephric fat stranding can be detected on chest CT," he said. "And correlation [between imaging and] laboratory results can be a predictor of acute kidney injury."
Common complication
Presenter Prof. Lorenzo Derchi of the University of Genoa in Italy also underlined how common renal involvement is in COVID-19 patients.
"Renal involvement -- defined as both urinary abnormalities and changes in kidney function -- has been described as present in up to 75% of COVID-19 cases," he said.
Derchi, a former president of the European Society of Radiology, described results from a study performed by nephrology colleagues at the University of Genoa. They investigated the effect of COVID-19 on 777 patients, and found the following:
- Acute kidney injury developed in 176 patients (22.6%).
- Of these 176, 79 (45%) showed acute worsening of preexisting chronic kidney disease.
- Of the 176 patients with acute kidney injury, 21 (12%) required kidney replacement therapy.
- Among patients who developed acute kidney injury, 111 died (63%).
- Patients with chronic kidney disease complicated by acute kidney injury had an almost double risk of death compared to patients without renal damage (hazard ratio, 1.79).
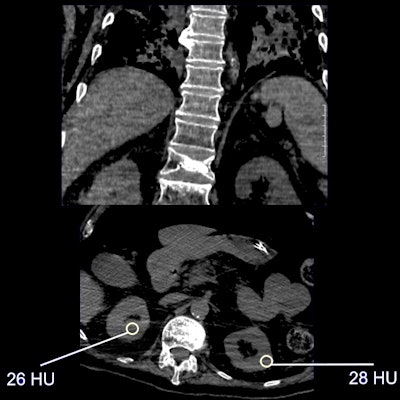 Nonenhanced CT shows renal parenchymal attenuation and edema and inflammation in COVID-19 patient. From: Li Z et al, Caution on Kidney Dysfunctions of COVID-19 Patients, medRxiv, 27 March 2020. This study found statistically significant lower CT value in COVID-19 patients; 27.3 HU (COVID-19 group) versus 33.2 HU (control group).
Nonenhanced CT shows renal parenchymal attenuation and edema and inflammation in COVID-19 patient. From: Li Z et al, Caution on Kidney Dysfunctions of COVID-19 Patients, medRxiv, 27 March 2020. This study found statistically significant lower CT value in COVID-19 patients; 27.3 HU (COVID-19 group) versus 33.2 HU (control group).The prevalence of kidney complications in COVID-19 patients highlights imaging's importance for supporting referring physicians, Derchi said. He offered three ways radiologists can do this:
- Be prepared to perform renal ultrasound evaluations in the emergency department for COVID-19 patients arriving with laboratory signs of renal insufficiency. Check for obstruction and signs of chronic kidney disease.
- Keep the kidneys in mind when reading chest CT exams, since the organ is often visible on caudal images. Look for perinephric fat stranding and renal density on unenhanced CT studies.
- Be aware of what renal clinicians expect from radiologists. "They want us to help them understand how COVID-19 may be affecting their patients' kidneys and to help them understand imaging findings," Derchi said.
Most importantly, according to Derchi, referring clinicians want radiologists to be available.
"They want us to be available for all their requests, even at bedside," he said. "[We're used to reading films remotely] but that may not be helpful enough to our colleagues, and in turn, their patients."