Prompt recognition of the complications from renal interventions is vital -- particularly given the potential threat to life -- and building up a greater understanding of early and delayed complications can allow radiologists to direct the management of patients, new research has found.
"The incidence of complications from renal interventions is expected to increase with the increasing incidence of renal pathologies," noted Drs. Jean S.Z. Lee, Jonathan Hall, and Tom Sutherland from the Medical Imaging Department, St Vincent's Hospital, Melbourne, Australia.
"The radiologist's role in detecting potential complications on imaging from renal interventions is, as such, more important than ever, especially with the general shift to less invasive approaches," they wrote in an article posted on 18 July by Insights into Imaging.
Knowledge of CT findings will enable the primary diagnosis of potential complications, the authors explained. An understanding of underlying risk factors may reduce complications from renal interventions, while early diagnosis of complications from renal intervention could improve the patient's prognosis.
Surgical complications
Potential vascular and nonvascular complications can arise from surgical, extracorporeal shock wave lithotripsy, radiotherapy, and radiological renal interventions, including percutaneous image-guided biopsy and drainage, the authors continued. Radiologists play a crucial role in recognizing and diagnosing post-renal intervention complications on CT scans, and their actions can significantly improve the patient's prognosis.
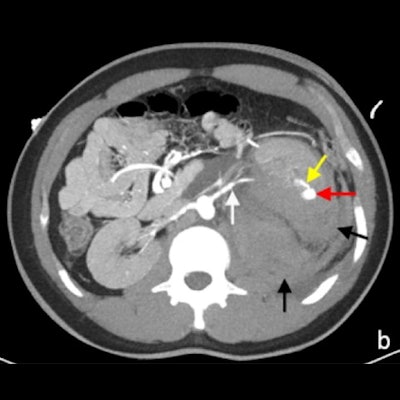
 (A) Arterial phase CT image of perinephric hematoma (white arrow) at the site of partial nephrectomy. The residual left kidney is indicated by the yellow arrow. (B) Active extravasation of contrast (white arrow) was confirmed on digital subtraction angiography. All figures courtesy of Dr. Jean S.Z. Lee and colleagues and Insights into Imaging.
(A) Arterial phase CT image of perinephric hematoma (white arrow) at the site of partial nephrectomy. The residual left kidney is indicated by the yellow arrow. (B) Active extravasation of contrast (white arrow) was confirmed on digital subtraction angiography. All figures courtesy of Dr. Jean S.Z. Lee and colleagues and Insights into Imaging.Open and laparoscopic radical nephrectomy is the gold standard in the management of large renal masses. For smaller lesions, nephron-sparing procedures such as partial nephrectomy or percutaneous therapies are increasingly favored.
"Early CT is indicated to assess the clinically suspected complications of surgery and to enable early management," stated Lee and colleagues. "Two main complications following nephrectomy requiring CT is hemorrhage and urinary leakage. Postoperative hemorrhage may arise from an unsecured artery, or days to weeks later due to the rupture of a pseudoaneurysm of an intrarenal artery."
The presence of a postoperative perinephric hematoma can be demonstrated by CT, ultrasound, or MRI, but the site of active hemorrhage is best demonstrated on a CT angiography or digital subtraction angiography (DSA).
Urological complications
The surgical management of urinary tract stones has evolved from open surgery to a range of minimally invasive procedures. With the exception of complex staghorn calculi, a range of minimally invasive techniques have been employed by urologists to treat urinary tract calculi, including extracorporeal shock-wave lithotripsy (ESWL), and ureteroscopy, flexible ureterorenoscopy, and percutaneous nephrolithotomy (PCNL).
The selection of each technique is influenced by the surgeon's experience, the nature of the stone burden, stone location, anatomy of the urinary tract, and patient preference.
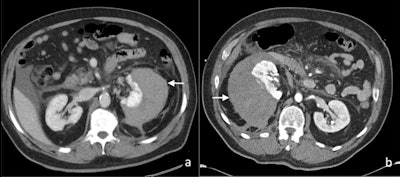 Axial contrast-enhanced CT images of (A) perinephric hematoma (white arrow), and (B) subcapsular hematoma (white arrow) postextracorporeal shock wave lithotripsy in two patients.
Axial contrast-enhanced CT images of (A) perinephric hematoma (white arrow), and (B) subcapsular hematoma (white arrow) postextracorporeal shock wave lithotripsy in two patients.One of the most common complications of ESWL is the formation of a perinephric or subcapsular hematoma, with an incidence of approximately 4%. The risk of a renal hematoma post-ESWL is significantly increased with increasing patient age, use of a therapeutic dose of low molecular weight heparin and the presence of an untreated urinary tract infection. The resultant compression of the kidney from the perinephric or subcapsular hematoma has been reported to cause systemic hypertension, also known as Page kidney.
Arteriovenous fistula occurs in up to 10%-15% of patients after percutaneous allograft biopsy in transplant kidney patients, with a lower rate of up to 10% following biopsy of native kidneys.
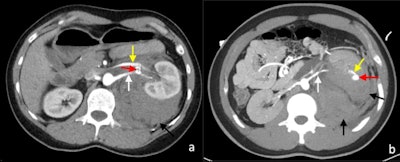 Postcontrast arterial phase axial CT images of vascular complications following nontargeted ultrasound-guided 14-gauge core biopsies of the left kidney in two patients. (A) Arteriovenous fistula. There is a fistulous connection (red arrow) between the left renal artery (white arrow) and the left renal vein (yellow) with associated early arterialised enhancement of the proximal left renal vein, medial to the arteriovenous fistula. There is an associated retroperitoneal hematoma (black arrow). (B) Arterial pseudoaneurysm. A small pseudoaneurysm (red arrow) arising from a segmental branch of the left renal artery (yellow arrow) is visualized as an adjacent small focus of rounded arterial enhancement (red arrow). The main left renal artery is also visible (white arrow). There is an associated left perinephric and retroperitoneal hematoma (black arrows).
Postcontrast arterial phase axial CT images of vascular complications following nontargeted ultrasound-guided 14-gauge core biopsies of the left kidney in two patients. (A) Arteriovenous fistula. There is a fistulous connection (red arrow) between the left renal artery (white arrow) and the left renal vein (yellow) with associated early arterialised enhancement of the proximal left renal vein, medial to the arteriovenous fistula. There is an associated retroperitoneal hematoma (black arrow). (B) Arterial pseudoaneurysm. A small pseudoaneurysm (red arrow) arising from a segmental branch of the left renal artery (yellow arrow) is visualized as an adjacent small focus of rounded arterial enhancement (red arrow). The main left renal artery is also visible (white arrow). There is an associated left perinephric and retroperitoneal hematoma (black arrows).Follow-up ultrasound Doppler shows that over 95% of fistulae detected were asymptomatic and about 95% of the fistulae spontaneously resolved at three months after biopsy. A small number of the patients develop hemodynamically significant bleeding and require treatment. Arteriovenous fistulas lead to early arterial enhancement of the involved vein, with similar enhancement to that of the abdominal aorta and renal arteries.
Tumor seeding
Tumor seeding along the percutaneous biopsy tract is rare, with an estimated incidence of approximately 1 in 3,000, according to the authors. Patients with papillary renal carcinoma, higher grade or stage tumor may be at higher risk of tumor seeding. Tumor seeding following surgery is also extremely rare, accounting for less than 0.1% of cases.
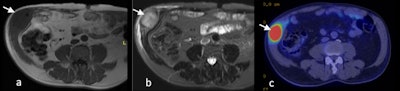 T1-weighted (A) and T2-weighted fat suppressed MRI (B) and PET-CT (C) images of transitional cell carcinoma recurrence within the right anterolateral abdominal wall scar (white arrow).
T1-weighted (A) and T2-weighted fat suppressed MRI (B) and PET-CT (C) images of transitional cell carcinoma recurrence within the right anterolateral abdominal wall scar (white arrow).Transitional cell carcinomas make up the majority of cases. Two cases of seeding from renal cell carcinoma along the cryoablation probe tract have been reported. Intraperitoneal metastases have also been reported following radiofrequency ablation. Port site metastases are associated with poor prognosis. The foci of tumor seeding typically demonstrate similar imaging characteristics to the primary tumor, the Melbourne team concluded.



















