The number of diagnostic nuclear medicine procedures (excluding PET) performed in France, Germany, Italy, Spain, and the U.K. rose by about 1% a year between 2007 and 2011, and France showed the highest level of growth in terms of patient numbers.
This year there will be around 5.2 million patient visits in European nuclear medicine markets, and therapy comprises a small proportion of the total patient studies at about 5%. Treatment for thyrotoxicosis accounts for more than half of these therapy procedures. The acceptance of some therapy applications, particularly radiosynoviorthesis, varies greatly across Europe.
Bone studies are likely to account for around 35% of procedures, and these have grown slowly over the period. Almost every center undertakes bone scanning. Endocrine procedures have also grown steadily, and thyroid examinations account for 95% of these studies. Together, thyroid and bone studies underpin the overall growth in procedure volumes.
 Mobile PET/CT units like this one in Geneva, Switzerland, are becoming more common sights. About 20 of them are now in operation across Europe. Image courtesy of Hôpitaux Universitaires de Genève (HUG).
Mobile PET/CT units like this one in Geneva, Switzerland, are becoming more common sights. About 20 of them are now in operation across Europe. Image courtesy of Hôpitaux Universitaires de Genève (HUG).
Cardiac studies account for about 18% of the remaining procedures, although the figure is higher if scans are counted but it is still relatively low compared with the U.S. Cardiac studies have held steady, although they face threats from echo, CT, MR, and PET/CT. A few centers have stopped the procedure, but this has been partly offset by rises elsewhere. Most European centers see fewer than 25 patients per week, and therefore interest in dedicated cardiac cameras is weaker in Europe than in the U.S.
The remaining studies are a mixture of winners and losers. Procedures that continue to lose out to other modalities include lung scans, most notably ventilation studies that switched to CT. Renal scans in which MRI and ultrasound are used and inflammation studies in which PET/CT is used are becoming a popular alternative. Lung and renal scanning each account for less than 10% of activity, and, at many sites, numbers are below the level for a daily service. New applications have captured some of the slack, most notably sentinel node imaging. Its share of applications is growing at about 1% per annum, which should see it capturing 10% of the examination volume by 2015. DaTSCAN, used to clarify the causes of tremor, has also exhibited strong growth.
About one-third of nuclear medicine departments now have access onsite to PET/CT. With about 20 mobile PET/CT units now in operation, another 30 plus centers have access to the technology. We have identified 520 PET and PET/CT systems operating in 2012 in the five major European markets. At approximately one system per million people, the U.K. falls way behind other leading European countries, where a PET/CT now serves closer to 500,000 people. Combining with data collected in 2010 for patient throughput, we estimate that in 2012 around a million studies will be performed in these markets. We will be refining this number later this year and looking at the types of studies undertaken.
The type and number of cameras a department operates gives a good indication of the likelihood of the centers taking on PET/CT in the future. A department with two or more cameras, one of which is a SPECT/CT, will hope to have PET/CT in the next five years. This would put PET/CT in two-thirds of departments by 2017.
Looking ahead, total nuclear scan numbers will continue to show only limited growth, and the trends seen over the last five years are likely to be replicated over the next five years. It takes around 10 years to introduce or replace an existing examination, so change will be slow.

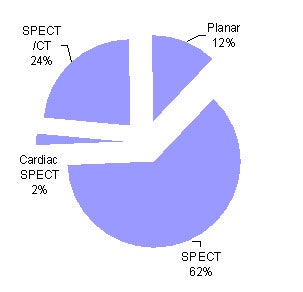
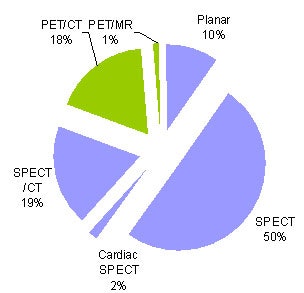 This series of charts shows the European study mix for nuclear medicine, including the types of camera operating in 2012. The third chart includes PET. All charts courtesy of Medical Options.
This series of charts shows the European study mix for nuclear medicine, including the types of camera operating in 2012. The third chart includes PET. All charts courtesy of Medical Options.During December 2011, the nuclear medicine camera installed base in the major markets was 2,837 installations at 1,279 sites. The total includes 2,020 cameras at public hospitals and 817 cameras at private hospitals/practices. The practices are a mixture of imaging and dedicated nuclear practices. Across the five largest countries, the number of installed systems has remained almost unchanged over the last seven years.
The European camera market is entirely replacement, most often with SPECT/CT. Planar cameras now account for less than 12% of the installed units. About 46% of departments have access to SPECT/CT.
The biggest future threat is the failure to attract new doctors into nuclear medicine. PET/CT will hopefully reverse this trend and underpin scintigraphy.
Anthony Stevens, PhD, is director of Medical Options, London (www.medicaloptions.co.uk). This article is based on results from the company's new study, Nuclear Medicine Europe 2012, which included more than 200 interviews across five major markets.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnie.com or AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.