Nearly all patients with negative results at screening virtual colonoscopy remain free of colorectal cancer five years later, concludes a new study in the European Journal of Radiology.
Results in more than 1,000 individuals screened with VC (also known as CT colonography or CTC) showed only one incident of colorectal cancer five years after the examination, as well as an additional 14 patients with advanced noncancerous lesions.
Several multicenter trials have validated CTC for detecting clinically significant polyps, and yields of advanced neoplasia are similar to those of colonoscopy, according to Dr. David Kim and colleagues from the University of Wisconsin in Madison. The technique's efficacy has led to its inclusion in the American Cancer Society's colorectal cancer screening guidelines.
"On the other hand, critics contend that widespread screening by CTC may lead to interval cancers that could be avoided if screened by colonoscopy," Kim and colleagues wrote. "They argue that the CTC selective polypectomy strategies where diminutive polyps are ignored and surveillance of isolated (one or two) 6- to 9-mm polyps is permissible result in many high-risk polyps and cancers that are not removed. Furthermore, such proponents assert that CTC is unable to detect many flat lesions, which may hold higher rates of high-grade dysplasia and invasive cancer" (Eur J Radiol, 23 December 2011).
If such hypotheses are correct, clinicians could expect to see an excessive number of interval cancers presenting clinically between CTC screening intervals, the group said. To examine the validity of those hypotheses, the researchers aimed to determine the rate of clinically presenting incident cancers over a five-year follow-up in a cohort of screening patients with negative CTC screening results.
The cohort included 1,050 asymptomatic individuals (mean age, 56.9 ± 7.4 years) with negative results at CTC over a 14-month period. From the original cohort of 1,179 asymptomatic individuals, 120 had positive CTC exams and were excluded. Also excluded were individuals with a history of inflammatory bowel disease, colorectal cancer, or polyposis syndrome, and those under surveillance for previously detected adenomas.
Patients underwent standard virtual colonoscopy exams beginning with a cathartic bowel preparation based on sodium phosphate, magnesium citrate, or polyethylene glycol. The tagging protocol included the administration of barium sulphate and diatrizoate. Cleansing was followed by automated colonic insufflation with CO2 (ProtoCO2l, Bracco Diagnostics).
The patients were scanned prone and supine on either an 8- or 16-detector-row CT scanner (LightSpeed series, GE Healthcare), with 1.25-mm collimation, a 1-mm reconstruction interval, 50-75 mAs, and 120 kVp. Among the 1,050 patients, 39 (3.7%) were excluded due to a lack of follow-up, leaving 1,011 patients followed for an average of 4.73 ± 1.15 years. The CTC-negative cohort included a single incident colorectal adenocarcinoma that presented at the routine screening interval, representing a crude incidence rate of 0.2 cancers per 1,000 person-years (95% confidence interval 0.00529 to 1.16421 per 1,000 person-years).
The interval cancer patient presented 25 months after negative CTC with "increased rectal urgency and altered stool habits," the authors noted. Workup revealed a stage II (T3, N0, M0) low rectal adenocarcinoma. A retrospective review of the CTC images revealed a questionable area of abnormality present on the index exam, "although the area is difficult to assess due to adjacent redundant tissues and the rectal balloon," the authors wrote, noting that the patient underwent curative resection and remains disease-free.
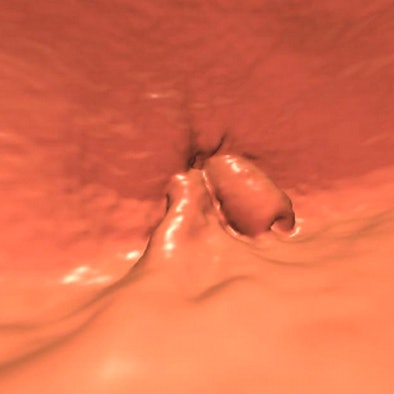 |
| A 65-year-old patient developed a low rectal adenocarcinoma, stage II (T3, N0), three years after a negative screening VC; original lesion seen in endoluminal view above. Image courtesy of Dr. Dustin Pooler and Dr. Perry Pickhardt. |
Among the patients who underwent luminal examination at follow-up, 14 had clinically significant lesions (14/368; 3.8%), including 11 who had an advanced adenoma based on size alone, and one case of tubulovillous histology. No advanced histology was detected, and no subcentimeter advanced histology was found. An additional five patients with six polyps 6- to 9-mm in size at interval screening, who opted for imaging surveillance, were identified, the authors reported. Finally, three patients had significant pericolonic gastrointestinal lesions, "including an appendiceal goblet cell carcinoid, an appendiceal mucinous tumor, and an ileo-cecal carcinoid with metastases to the liver," Kim and colleagues reported.
Clinically presenting colorectal adenocarcinoma is rare in the five years following negative screening CTC, they concluded.
Concerns have arisen over the potential for incident cancers because polyps smaller than 6 mm are ignored at CTC, the authors noted. Yet most diminutive lesions "never progress to cancer or harbor cancer (0.03% of diminutive polyps)," they argued. "The few potentially important polyps in this group can be identified by demonstrating interval growth as they pass the 6-mm threshold on future routine screening examinations set at five-year intervals."
CTC's 6-mm threshold greatly diminishes the number of polypectomies, while maintaining cancer yields equivalent to those of conventional optical colonoscopy, they stated.
Critics fear that VC could leave too many small cancers inside the patient; in particular, Rex et al reported that 5% of negative CTC patients may harbor high-risk adenoma findings. "However, it is important to realize that more than 90% of these cases will consist of patients with only three or more diminutive tubular adenomas, which are of uncertain but doubtful importance," Kim and colleagues stated.
"The results of our study strongly argue against the clinical relevance of these debated concerns and suggest that the five-year interval between negative CTC screening examinations is a safe practice," they wrote, noting the presence of only a single incident symptomatic cancer in the cohort. "This colorectal cancer outcome mirrors the results seen at colonoscopy screening -- despite the markedly different polyp harvesting strategies and the underlying difference in technique," added the authors, citing the results of Imperiale et al, which found only one interval cancer five years after negative colonoscopy screening.
The crude cancer incidence rate in the study's negative CTC cohort (0.2 cancers/1,000 person-years) "is substantially lower than the rates observed in colonoscopic surveillance cohorts where rates range from 1.7 to 2.4 cancers per 1,000 person-years," they wrote. This difference suggests that a CTC-negative cohort is at substantially lower risk compared to a colonoscopy surveillance cohort whose participants have an advanced lesion removed at colonoscopy and are then followed, according to Kim and colleagues.
"The lack of high-grade dysplasia (or malignant foci) among these advanced lesions in our study adds to the mounting evidence that transformation of these lesions occurs over the span of many years," they wrote. "These findings reinforce the relative indolent nature of diminutive adenomas. However, the outcomes do point out that programmatic screening compliance is required in order to detect these lesions."