The emergence of 3D printed models costing around €20 each represents a sustainable way of enhancing surgical planning and medical communication, according to a global research team.
"The economic accessibility of these models may broaden their adoption, especially in budget-constrained environments," noted Dr. Pedro Zapata, a radiologist at Hospital San Felipe de Jesús and a PhD candidate at Tecnológico de Monterrey, School of Medicine and Health Sciences, Monterrey, Mexico, and colleagues. "This approach, backed by open technologies and cost-effective 3D models, holds the promise of democratizing access to medical innovation and advancing surgical care on a global scale."
At RSNA 2024 in Chicago, Zapata displayed his 3D-printed model for preoperative planning in osteosarcoma surgery. This project, presented at the RSNA 3D SIG Showcase, highlights how 3D technology can enhance surgical outcomes and personalize patient care. Each of the models on display was a testament to the innovation and creativity in 3D printing for medicine, he said.
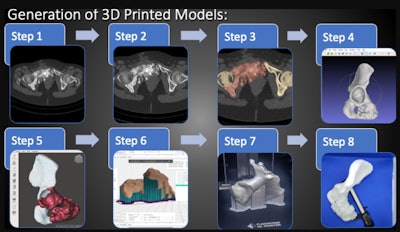 Sequential steps involved in the generation of 3D printed models. Step 1: Selection of CT and MRI studies. Step 2: Radiologist's analysis and fusion of CT and MRI modalities. Step 3: Segmentation using 3D Slicer. Step 4: Refinement with MeshLab. Step 5: Preparation and editing with Meshmixer. Step 6: 3D printing preparation with FlashPrint. Step 7: 3D printing using FDM Printer and PLA material. Step 8: Measurement with millimetric caliper. Courtesy of Dr. Pedro Zapata et al and ESR EPOS database.
Sequential steps involved in the generation of 3D printed models. Step 1: Selection of CT and MRI studies. Step 2: Radiologist's analysis and fusion of CT and MRI modalities. Step 3: Segmentation using 3D Slicer. Step 4: Refinement with MeshLab. Step 5: Preparation and editing with Meshmixer. Step 6: 3D printing preparation with FlashPrint. Step 7: 3D printing using FDM Printer and PLA material. Step 8: Measurement with millimetric caliper. Courtesy of Dr. Pedro Zapata et al and ESR EPOS database.
So how is it done? The aim is to develop innovative and budget-friendly solutions, specifically designed to elevate surgical assessments in financially restricted environments, according to Zapata. Leveraging open-source software like 3D Slicer, MeshLab, Meshmixer, FlashPrint, and CloudCompare, fused deposition modeling (FDM) printing technology, and PLA (also known as polylactic acid or polylactide) as printing material, the focus is on optimizing costs in crafting 3D printed models, aligning with principles of open access and collaborative scientific practices.
"3D printed models are not just practical solutions; they represent an extension of specialized interpretation for radiologists," he explained. "These models, intricately developed through segmentation, editing, and printing processes, transcend language limitations."
The incorporation of various colors enhances visual communication within the medical team, adding depth to clinical practice and highlighting the transformative potential of 3D printed models in interpreting and conveying radiological findings, he added.
Methodology used
The selection of CT and MRI studies adheres to specific criteria, with clearly defined optimal requirements for segmentation. The protocol involves the analysis of CT and MRI by a radiologist, and through a fusion of these two modalities, the radiologist will perform segmentation utilizing 3D Slicer, followed by MeshLab for refinement, Meshmixer for preparation and editing, and FlashPrint for 3D printing preparation.
Each step of the protocol is crucial to ensure the highest fidelity possible in the 3D-printed model, the researchers pointed out. The 3D models are printed using an FDM 3D printer, Creator 3 FlashForge PLA in multiple colors.
"After printing, the models are measured with a millimetric caliper, followed by a CT scan," they said. "The DICOM files of the 3D printed model CT are segmented using the same process as before, resulting in a new 3D STL model. A meticulous comparative analysis between CT-generated models and 3D printed models is conducted using CloudCompare."
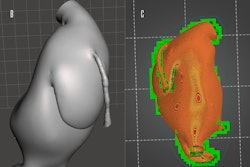
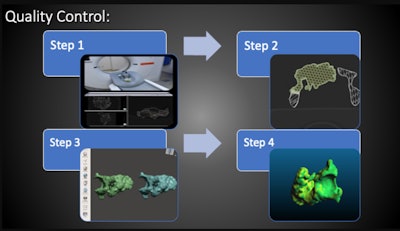 Sequential steps involved in quality control. Step 1: CT scan of printed model. Step 2: Segmentation of 3D-printed model CT with 3D Slicer. Step 3: Comparative analysis with overlaying of 3D STL files. Step 4: Comparative analysis with CloudCompare overlay with color map. Courtesy of Dr. Pedro Zapata et al and ESR EPOS database.
Sequential steps involved in quality control. Step 1: CT scan of printed model. Step 2: Segmentation of 3D-printed model CT with 3D Slicer. Step 3: Comparative analysis with overlaying of 3D STL files. Step 4: Comparative analysis with CloudCompare overlay with color map. Courtesy of Dr. Pedro Zapata et al and ESR EPOS database.
To estimate the cost of the 3D-printed models, Zapata and colleagues developed a formula considering the cost of electricity in Mexico and the cost of PLA material, with an additional factor for printer wear-and-tear: Cost per print = (Cost of printer per hour + maintenance cost per hour + electricity cost) × number of printing hours + (cost of printing material per gram × grams used per print); CpP = 17.92H + 0.7g.
The time required from analyzing DICOM images to obtaining a 3D-printed model varies for each case and is heavily influenced by the complexity and size of the model, they noted. "On average, this process takes approximately 24 hours, with 18 hours dedicated to 3D printing and the remaining time allocated to segmentation, editing, and slicing. The amount of material used also tends to vary, averaging around 300 grams."
Showcasing significant similarities in size and shape, they compare the CT-printed 3D tumor models with the "original" STL models. Despite variations in scalar fields and distributions, the models maintain overall coherence. These slight variations, however, do not have a significant impact on their usability in surgical evaluation, even as a foundation for developing personalized cutting guides or implants.
The average cost per 3D printed model is estimated at $23 (€20.9). This estimation does not include payment for the radiologist's work, Zapata emphasized.
 Series of images demonstrating the clinical impact of 3D printing technology in a pelvic osteosarcoma case. The first image shows the preoperative x-ray with the osteosarcoma involving the left pelvis. The central panel illustrates the 3D printed model used for preoperative planning, along with the resected specimen showing the tumor margins. The third panel displays the postoperative x-ray, highlighting the reconstruction with cadaveric bone grafts and a custom implant. Courtesy of Dr. Pedro Zapata and presented at RSNA 2024.
Series of images demonstrating the clinical impact of 3D printing technology in a pelvic osteosarcoma case. The first image shows the preoperative x-ray with the osteosarcoma involving the left pelvis. The central panel illustrates the 3D printed model used for preoperative planning, along with the resected specimen showing the tumor margins. The third panel displays the postoperative x-ray, highlighting the reconstruction with cadaveric bone grafts and a custom implant. Courtesy of Dr. Pedro Zapata and presented at RSNA 2024.
For further details, go to the full ECR 2024 exhibit on the EPOS website of the ESR (epos.myesr.org/poster/esr/ecr2024/C-12066). The co-authors were D.B. Avendano, S. Cardona-Huerta, J. Tamez, M.A. Marino, and C. Sofia.