Modern 3D printing techniques can be of great value in the management of patients with aortic wall disease, but implementation requires technical knowledge and a complex understanding of the anatomy and pathology and the surgical treatment options available, according to researchers.
The results with 3D printing so far have been promising, but further investigation and more documented studies regarding the topic are needed to provide more insight, stated Dr. Sabin Cristian Radu and colleagues from the University of Medicine and Pharmacy "Carol Davila" in Bucharest, Romania. The team has shared its experiences implementing the technology into its workflow and highlighted potential difficulties and setbacks.
"The possibility of custom-made, patient-specific implants and tools for preoperative or educational purposes has shown great value in allowing us to visualize complex anatomy, aid in surgical planning, improve training, and lower surgery time," the group noted.
 The model was used to provide an initial understanding of the actual size of the aneurysm and the position and course of both coronary arteries. Total printing time was around 7.5 hours. All figures courtesy of Dr. Sabin Cristian Radu, Prof. Bogdan Popa, et al and presented at ECR 2024.
The model was used to provide an initial understanding of the actual size of the aneurysm and the position and course of both coronary arteries. Total printing time was around 7.5 hours. All figures courtesy of Dr. Sabin Cristian Radu, Prof. Bogdan Popa, et al and presented at ECR 2024.
A wide range of readily available software programs and 3D printers are now commercially available, and a range of factors must be considered when implementing a 3D printer in a vascular surgical environment. Fused deposition modeling (FDM) or stereolithography (SLA) are the most common technologies used, and both have their strengths and weaknesses. The Bucharest group has worked only with an FDM printer, but the plan is to add a resin printer to their setup.
"Resolution of the 3D printer plays an important aspect particularly in small lumen vessels, for the aorta is of less importance. Of all the materials available for commercial 3D printing, finding a suitable one for reproducing a vascular model is no easy task. The price range of 3D printers is rather large, but that is only the initial investment, the cost of materials and maintenance should also be considered in the long term," the researchers noted.
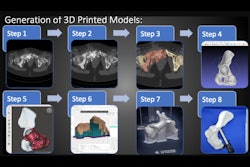
In a poster exhibited at ECR 2024, they proposed a step-by-step approach to the printing process of aortic models, starting with image acquisition, patient selection, image postprocessing, and 3D printing, before ending with printed object postprocessing and preoperative planning.
For a smooth 3D printing process, the images procured by CT angiography should have no image artifacts or as low as possible, optimal contrast for the region of interest, isotropic voxel resolution, and low noise. An image thickness between 0.5-1.5 mm is desirable. Patients who require elective surgery are the most suitable, the team stated.
The DICOM format does not allow users to directly print, so it's essential to separate the structures of interest from the raw data and transform it into a format accessible to 3D printers, the most notable one being stereolithography (STL). The main tool the Bucharest group uses for segmentation is 3D Slicer, a free, open-source, cross-platform software.
After exporting data from the PACS, preferably anonymized, they import the data set to 3D Slicer and extract a reconstruction of the vascular structure of interest consisting of intraluminal contrast. "This is called a segmentation (isolation of anatomical structures from their surroundings)."
There are various tools useful in achieving this task, either manually or using certain semiautomated techniques (thresholding, edge detection, region segmentation, atlas-based) or automated techniques (AI, supervised or unsupervised) or a mix of tools. All the models were made using a combination of semiautomatic techniques and then manual editing.
 Fusiform aneurysm measuring about 7/7/10 cm AP/TR/CC with mural thrombus measuring 2.5 cm and small dissection (false lumen measuring 3.5/1.2 cm). Periaortic hematoma was noted measuring 1.7 cm; iliac arteries with normal caliber and no active bleeding reported. The model was used to assess infrarenal neck angle and shape, position, and course of inferior mesenteric artery.
Fusiform aneurysm measuring about 7/7/10 cm AP/TR/CC with mural thrombus measuring 2.5 cm and small dissection (false lumen measuring 3.5/1.2 cm). Periaortic hematoma was noted measuring 1.7 cm; iliac arteries with normal caliber and no active bleeding reported. The model was used to assess infrarenal neck angle and shape, position, and course of inferior mesenteric artery.
The STL data provided by 3D slicer is further enhanced using Meshmixer (Autodesk Inc.) by smoothing the model and subtracting the luminal volume to provide a hollow model. There are a few aspects that need to be considered in post-processing of the 3D structure before printing: eliminating nonmanifold surfaces or edges, repairing the mesh by filling unwanted holes, removing or reconnecting mesh islands to the main mesh, ensuring mesh quality so that printing resolution correlates to image resolution, remeshing and eliminating unnecessary triangles from the mesh, and selecting the desired wall thickness.
All the group's models are remeshed (reducing the mesh varying between 20%-30%), for a lower triangle count and faster processing, but preserving shape and size (life-sized models), smoothed out (10% factor), then fixed using the Analysis tool, ensuring the mesh quality with the Flat fill function of various defects listed above. The wall thickness was arbitrarily set at 0.4 mm, respectively 1 mm while hollowing the model, and the ends were discarded using the plane cut method.
All the prints are done on the Prusa Mini at 0.2 mm quality (layer height), as this is less time-consuming but still retains a decent aspect, with variable layer height (0.1-0.2 mm) on areas with more details or difficult overhangs and curvature.
"The printing speed and extruding temperatures used were the recommended ones for the specific material. Infill values between 0%-15% were used having a more transparent finish for lower values but less resistance and structural integrity. Supports were automatically generated and manually edited to assure a smooth printing process," the researchers added.
After cooling the print supports were gently removed using different cutting tools and pliers. Some internal parts could not be removed entirely because of difficult access. No sanding or physical smoothing was done so as to not reduce the transparency of the prints. Salt annealing (transformation of amorphous polymers into the semicrystalline structure) was tried using a heat convection oven at a temperature of 110°C and 150°C for 30 to 45 minutes with little success in achieving better transparency and the resulting deformities being rather significant.
"Utilizing an open-source software setup and a desktop 3D printer allowed us to produce vascular models capable of being important teaching tools regarding endovascular/surgical procedures in aortic aneurysms, pseudoaneurysms or dissections," Radu and colleagues wrote.
The choice of procedure, stents, and grafts utilized was made using the CT images, but the models were used after to better assess the anatomy and to build confidence in the selected surgical procedure. Regarding the transparency of the models perhaps an SLA printer will have better results, the models obtained being at best translucent at the lowest values of infill that still provided structural integrity. Also, SLA technology would reduce part of the internal supports that are difficult to remove.
"Although flexible models were obtained, none were transparent enough or watertight. Nonetheless, this setup can be a minimal cost stepping stone into 3D printing aortic wall models," the group concluded.
The coauthors of the presentation were Prof. Bogdan Popa, Dr. Costin Aurelian Minoiu, and Dr. Marius-Adrian Ali. You can access the full exhibit on the EPOS website of the European Society of Radiology.