F-18 prostate-specific membrane antigen (PSMA) PET/CT is having an important impact on patient care and guiding treatment decisions in prostate cancer, but to accurately diagnose disease, it’s crucial to bear in mind some interesting quirks of the modality, Irish researchers have reported.
“PSMA is a transmembrane glycoprotein that is overexpressed in the majority of prostate cancers. This overexpression enables the identification of prostate cancer and metastases using radiolabelled small molecules that bind with high affinity,” noted Dr. Jonathan Hunter and colleagues in the radiology department at the Mater Misericordiae University Hospital in Dublin.
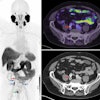
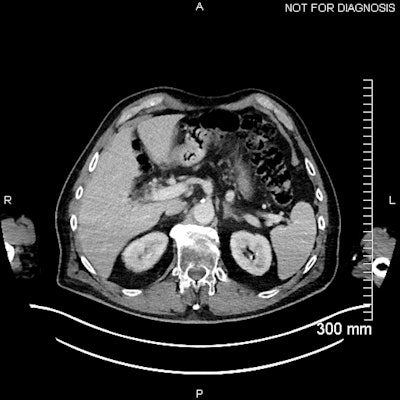
 (Above) Fused axial image demonstrates uptake in the celiac ganglia. (Below) Corresponding CT scan. The celiac ganglia are visible. All figures courtesy of Dr. Jonathan Hunter, Dr. Jane Burns, and Prof. Martin O’Connell and presented at ECR 2025.
(Above) Fused axial image demonstrates uptake in the celiac ganglia. (Below) Corresponding CT scan. The celiac ganglia are visible. All figures courtesy of Dr. Jonathan Hunter, Dr. Jane Burns, and Prof. Martin O’Connell and presented at ECR 2025.
PSMA PET/CT has become an important diagnostic tool in the primary diagnosis and staging prostate cancer, as well as in detecting biochemical recurrence after curative treatment and in metastasis-directed therapy.
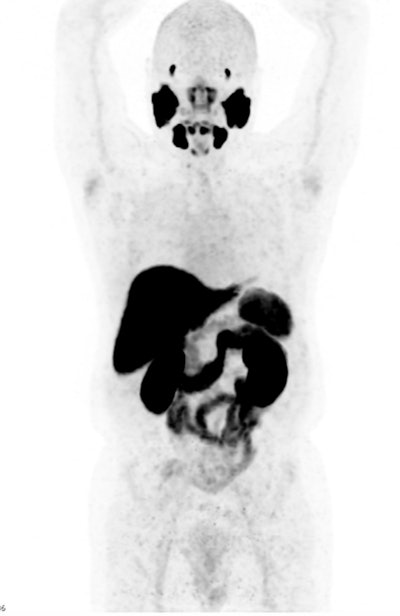 Normal radiotracer distribution for F-18-PSMA.
Normal radiotracer distribution for F-18-PSMA.
“It has led to a shift away from traditional algorithms, introduced the field of theranostics, and brought attention to as many uncertainties as it has advancements,” they explained in an e-poster at ECR 2025. “The advent of PSMA PET/CT has highlighted the limitations of conventional staging methods and may even have a greater influence on patient treatment and allow clinicians to make more informed treatment decisions.”
To accurately interpret nuclear medicine studies, a knowledge of the normal physiological distribution of the radiotracer is required. PSMA expression is present in normal prostatic tissue, though at a low level, and can also be found in the salivary and lacrimal glands, nasal cavity, larynx, liver, spleen, intestines, kidneys, and sympathetic ganglia, the authors pointed out.
 The first F-18-PSMA-1007 PET study was performed at the Mater in April 2022. The patient had been diagnosed with prostate cancer more than a decade earlier, having multiple nodal, lung, and bone metastases. Despite ongoing treatment with gonadotrophin-releasing hormone agonists, his prostate-specific antigen (PSA) was continually rising.
The first F-18-PSMA-1007 PET study was performed at the Mater in April 2022. The patient had been diagnosed with prostate cancer more than a decade earlier, having multiple nodal, lung, and bone metastases. Despite ongoing treatment with gonadotrophin-releasing hormone agonists, his prostate-specific antigen (PSA) was continually rising.
The physiological uptake of PSMA ligands in various normal tissues is an important pitfall in PSMA-targeted imaging, they continued. In particular, uptake in sympathetic trunk ganglia can pose challenges to nuclear medicine readers and may mimic lymph nodes. Also, cervical chain and coeliac ganglia may demonstrate higher uptake with F-18 PSMA.
“An interesting finding noted in PSMA PET/CT has been the emergence of benign, focal bone uptake,” Hunter and colleagues told ECR attendees. “It has been suggested that this uptake in benign lesions occurs more frequently with F-18-PSMA compared with gallium-68 (Ga-68)-PSMA. This is important to be aware of while interpreting F-18-PSMA PET/CT, as this can be easily mistaken for metastases, which may subsequently result in erroneously up-staging a patient.”
The phenomenon of a “superscan” was first described in 1975 for bone scintigraphy and is considered to be widespread, intense, and largely symmetrical uptake of the osseous radiotracer, typically accompanied by minimal or absent tracer accumulation in the urinary system and soft tissues. This is generally a finding that occurs in technetium-99m hydroxymethylene diphosphonate (Tc-99m HMDP) bone scans, but there have been some reports of the “superscan” appearance with PET/CT, as well as some evidence of it occurring with Ga-68 PSMA PET.
!['Superscan' appearance for [F-18]-PSMA-1007.](https://img.auntminnieeurope.com/mindful/smg/workspaces/default/uploads/2025/04/2025-04-24-mol-insider-figure-11.Qcm0S9jffh.png?auto=format%2Ccompress&fit=max&q=70&w=400) "Superscan" appearance for [F-18]-PSMA-1007.
"Superscan" appearance for [F-18]-PSMA-1007.
Uptake in renal lesions, particularly primary renal malignancies, has been described (see Journal of Cancer Research and Clinical Oncology 2022 June;148[6]:1299-311). Also, PSMA PET/CT has proved very useful in the evaluation of disease discordance.
You can read the full ECR poster here. The co-authors were Jane Burns, Michael Fitzsimons, David Caldwell, Martin O'Connell, and Paddy Gilligan.