Metabolic tumor volume (MTV) is a relatively accurate predictor of outcomes in pleural mesothelioma treated with immunotherapy, according to a Norwegian-led PET/CT study. The researchers also found that high maximum standardized uptake value (SUVmax)/peak is not associated with a worse outcome in this patient group.
"The lack of association between high SUVmax/peak and poor outcomes contrasts with previous research on patients treated with chemotherapy, which might be due to the introduction of immunotherapy as a new treatment modality," noted first author Dr. Solfrid Maria Thunold, a doctoral candidate in the department of oncology at Oslo University and the department of cancer genetics, Institute for Cancer Research, Oslo University Hospital.
An early decline in SUVmax/peak is associated with an objective response and may precede radiological changes, they wrote in an article posted on 12 August in the European Journal of Nuclear Medicine and Molecular Imaging (EJNMMI).
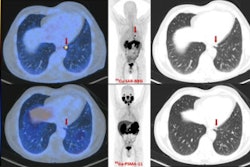
![Example of a patient with a decline in metabolic tumor volume (MTV) and F-18 FDG uptake as early as the week-five PET scan, which was followed by a long-term objective tumor response. Comparative imaging from baseline (top row) and week five (bottom row). To the left, axial CT images; in the middle, axial PET/CT images; and to the right, the maximum intensity projection (MIP). The PET images are observed within a 0-10 SUV window. The patient was classified as having stable disease at the first CT response assessment, before developing partial response at the week-12 CT scan according to the modified Response Criteria in Solid Tumours (mRECIST) and immune RECIST. While the patient had stable disease at the week-5 CT scan, PET/CT already showed a reduction in MTV and a decline in [F-18] FDG uptake in the tumor. The treatment was discontinued after seven months due to intolerable toxicity. The patient is still under follow-up 20 months after the start of the treatment. All figures courtesy of Dr. Solfrid Thunold et al and EJNMMI.](https://img.auntminnieeurope.com/files/base/smg/all/image/2024/08/2024_08_15_mol_insider_Figure_6.66bcf14cd240e.png?auto=format%2Ccompress&fit=max&q=70&w=400) Example of a patient with a decline in metabolic tumor volume (MTV) and F-18 FDG uptake as early as the week-five PET scan, which was followed by a long-term objective tumor response. Comparative imaging from baseline (top row) and week five (bottom row). To the left, axial CT images; in the middle, axial PET/CT images; and to the right, the maximum intensity projection (MIP). The PET images are observed within a 0-10 SUV window. The patient was classified as having stable disease at the first CT response assessment, before developing partial response at the week-12 CT scan according to the modified Response Criteria in Solid Tumours (mRECIST) and immune RECIST. While the patient had stable disease at the week-5 CT scan, PET/CT already showed a reduction in MTV and a decline in [F-18] FDG uptake in the tumor. The treatment was discontinued after seven months due to intolerable toxicity. The patient is still under follow-up 20 months after the start of the treatment. All figures courtesy of Dr. Solfrid Thunold et al and EJNMMI.
Example of a patient with a decline in metabolic tumor volume (MTV) and F-18 FDG uptake as early as the week-five PET scan, which was followed by a long-term objective tumor response. Comparative imaging from baseline (top row) and week five (bottom row). To the left, axial CT images; in the middle, axial PET/CT images; and to the right, the maximum intensity projection (MIP). The PET images are observed within a 0-10 SUV window. The patient was classified as having stable disease at the first CT response assessment, before developing partial response at the week-12 CT scan according to the modified Response Criteria in Solid Tumours (mRECIST) and immune RECIST. While the patient had stable disease at the week-5 CT scan, PET/CT already showed a reduction in MTV and a decline in [F-18] FDG uptake in the tumor. The treatment was discontinued after seven months due to intolerable toxicity. The patient is still under follow-up 20 months after the start of the treatment. All figures courtesy of Dr. Solfrid Thunold et al and EJNMMI.
Pleural mesothelioma has a dismal prognosis, with a median overall survival of approximately one year, and given the wide variations in disease progression and the scarcity of prognostic and predictive biomarkers, selecting the most effective therapeutic approach is difficult, the authors explained. In the context of multimodal treatment comprising chemotherapy, surgery, and possibly radiation therapy, F-18 FDG-PET/CT serves as a standard assessment tool for evaluating disease extension, but it is not routinely used for inoperable patients.
"The introduction of immunotherapy has revealed several unique tumour response patterns, some of which may be difficult to detect using standard radiological imaging due to their lack of volumetric changes," they stated. "Moreover, differentiating between progressive disease and pseudoprogression poses a challenge."
The ability of F-18 FDG-PET/CT to depict the metabolic microenvironment, in addition to anatomical structures, may be beneficial in evaluating early response to immunotherapy, the authors added.
 Example of a patient with a pseudoprogression. An initial increase in tumor volume and MTV and a decline in F-18 FDG uptake at week five was followed by a long-term objective tumor response/disease control. Comparative imaging from baseline (top row), week five (middle row), and year one (bottom row). To the left, axial CT images; in the middle, axial PET/CT images; and to the right, the MIP. The PET images are observed within a 0-10 SUV window. The patient was classified as having progressive disease at the first CT response assessment, before developing stable disease at week 12 and partial response at the week 18 CT scan according to mRECIST and immune RECIST. At week five, the PET/CT showed an increase in MTV, while F-18 FDG uptake (SUVmax and SUVpeak) has started to decline. At the one-year follow-up PET/CT, there is a notable change, with a visible reduction in tumor size, MTV, and F-18 FDG uptake. This corresponded with clinical performance status, which was reduced at week five and improved from week 12 and onwards. The patient died due to disease progression two years after the start of the treatment.
Example of a patient with a pseudoprogression. An initial increase in tumor volume and MTV and a decline in F-18 FDG uptake at week five was followed by a long-term objective tumor response/disease control. Comparative imaging from baseline (top row), week five (middle row), and year one (bottom row). To the left, axial CT images; in the middle, axial PET/CT images; and to the right, the MIP. The PET images are observed within a 0-10 SUV window. The patient was classified as having progressive disease at the first CT response assessment, before developing stable disease at week 12 and partial response at the week 18 CT scan according to mRECIST and immune RECIST. At week five, the PET/CT showed an increase in MTV, while F-18 FDG uptake (SUVmax and SUVpeak) has started to decline. At the one-year follow-up PET/CT, there is a notable change, with a visible reduction in tumor size, MTV, and F-18 FDG uptake. This corresponded with clinical performance status, which was reduced at week five and improved from week 12 and onwards. The patient died due to disease progression two years after the start of the treatment.
Patients receiving ipilimumab and nivolumab +/- telomerase vaccine in second line were included in the study. F-18 FDG-PET/CT was obtained at baseline (n = 100) and at week five (n = 76). The researchers evaluated MTV and SUVpeak in relation to survival outcomes, and they assess differences in MTV, total lesion glycolysis (TLG), SUVmax, and SUVpeak between patients exhibiting an objective response, defined as either partial response or complete response according to the modified Response Criteria in Solid Tumours (mRECIST) and immune RECIST (iRECIST), and nonresponders, defined as either stable disease or progressive disease as their best overall response.
Their analysis revealed significant associations of MTV with overall survival (OS) and progression-free survival (PFS), while multivariate analysis showed a significant association with OS only. While SUVpeak was not significantly associated with OS or PFS in univariate analyses, it was significantly associated with OS in multivariate analysis, and objective responders had significant reductions in TLG, SUVmax, and SUVpeak at week five.
"Some results aligned with our expectations, while others did not," Thunold told AuntMinnieEurope.com on 14 August. "The lack of association between high SUVmax/peak and poor outcomes was unexpected. It was also interesting to observe a decline in SUV metrics as early as week five among the objective respondents."
Further studies are needed to investigate the role of FDG-PET in pleural mesothelioma patients treated with immunotherapy, she added.
The researchers are currently evaluating the dual time-point PET data from the Nivolumab and Ipilimumab Plus/minus UV1 vaccination (NIPU) study. "By extracting SUV metrics from biopsy sites at baseline and after five weeks of treatment and combining this with RNA sequencing, we aim to explore potential associations between SUV dynamics and tumor composition, to see if this can give information about immunological changes in the tumor," she noted.
You can read the full open-access EJNMMI paper here: https://link.springer.com/article/10.1007/s00259-024-06853-0.