An experimental PET radiotracer that targets gastrin-releasing peptide receptors (GRPR) on prostate cancer cells has shown promise in a phase II clinical trial in Australia.
Nuclear medicine physicians at St. Vincent’s Hospital in Sydney tested the tracer in 25 patients and found that it detected disease recurrence in 44% of patients who were negative on prostate-specific membrane antigen (PSMA) PET scans.
“This study confirmed that targeting of alternative receptors to PSMA in prostate cancer may add diagnostic value and have an impact on management,” wrote senior author Dr. Louise Emmett and colleagues. The study was published on 1 August in the Journal of Nuclear Medicine.
PSMA-PET scans have revolutionized patient management when prostate cancer recurs in patients after primary therapy, yet negative PSMA-PET results remain common at lower prostate-specific antigen (PSA) levels, the authors explained.
GRPR is also overexpressed in many prostate tumors and to that end, researchers developed a copper-64-labeled ligand that binds to GRPR receptors called sarcophagine-bombesin (SAR-BBN). So far, Cu-64 SAR-BBN PET/CT has only been proven effective in animal studies and a first-in-human study.
Of the 25 patients enrolled in this trial, 96% (24/25) had prior radical prostatectomy, 4% (1/25) had brachytherapy, and 64% (16/25) had salvage radiotherapy. The median prostate-specific antigen (PSA) level at imaging with Cu-64 SAR-BBN was 0.69 ng/mL. At enrollment, 76% (19/25) of participants had negative PSMA-PET results and 24% (6/25) had equivocal PSMA PET results.
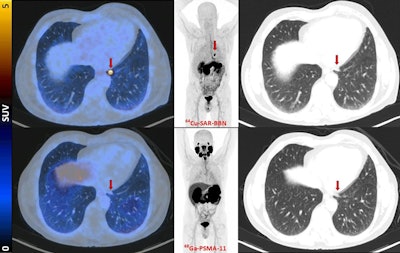 Fused PET/CT, maximum-intensity projection PET, and lung-windowed CT images (from left to right) from Cu-64 SAR-BBN (top row) and Ga-68 PSMA-11 (bottom row) PET/CT study of patient demonstrating left subpleural lesion (arrows, SUVmax of 10 at 1 hour) that showed Cu-64 SAR-BBN uptake but no Ga-68 PSMA-11 uptake. PSA was 1.84 ng/mL at time of imaging. This patient underwent lobectomy, with histopathology demonstrating metastatic prostate cancer.Image courtesy of the Journal of Nuclear Medicine
Fused PET/CT, maximum-intensity projection PET, and lung-windowed CT images (from left to right) from Cu-64 SAR-BBN (top row) and Ga-68 PSMA-11 (bottom row) PET/CT study of patient demonstrating left subpleural lesion (arrows, SUVmax of 10 at 1 hour) that showed Cu-64 SAR-BBN uptake but no Ga-68 PSMA-11 uptake. PSA was 1.84 ng/mL at time of imaging. This patient underwent lobectomy, with histopathology demonstrating metastatic prostate cancer.Image courtesy of the Journal of Nuclear Medicine
According to the findings, Cu-64 SAR-BBN-avid disease was identified in 44% (11/25) of participants. Of patients with positive Cu-64 SAR-BBN PET/CT results, 37% (3/11) had prostate bed recurrence, 46% (5/11) had pelvic node disease, and 27% (3/11) had distant disease (lung and bone).
“These findings support the potential role of 64Cu-SAR-BBN PET/CT as a second-line imaging modality for [biochemically recurrent] prostate cancer,” the group wrote.
Ultimately, negative PSMA-PET results remain common at lower PSA levels at which patients are curable with salvage therapy, and thus, additional diagnostic tools beyond PSMA-PET that further stratify patients who have distant disease would be clinically valuable, the authors suggested.
“The promising results from this study suggest that larger trials may be warranted to further evaluate benefit,” the group concluded.
The full study is available here.