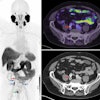
FDG-PET/CT imaging can reduce unnecessary surgeries to remove residual neck cancer in patients who have undergone chemoradiotherapy, according to a Dutch study.
In an analysis of treated patients with head and neck squamous cell carcinoma (HNSCC), integrating FDG-PET/CT helped select patients for surgery and ruled it out in a significant number of others, noted lead author Dr. Arash Navran of the Netherlands Cancer Institute in Amsterdam.
"FDG-PET/CT improved the accuracy of selection of patients for [salvage neck dissection] and decreased unnecessary [salvage neck dissection] in considerable number of patients," the team wrote in a paper published on 28 June in Radiotherapy and Oncology.
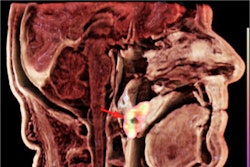
After primary treatment with chemoradiotherapy, up to 40% of patients with HNSCC may still have residual disease in the neck. Salvage neck dissection (SND) is performed to remove the cancer, with MRI or CT and ultrasound typically used to identify the disease.
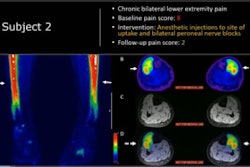
FDG-PET/CT is being increasingly used to evaluate how patients respond to treatment; however, few studies have assessed which imaging method may be superior for selecting patients for surgery, the investigators noted.
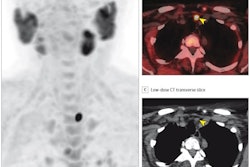
To that end, the researchers analyzed records on 908 consecutive patients with node-positive HNSCC treated with chemoradiotherapy at their institution. The primary endpoint of the study was the positive predictive value (PPV) of FDG-PET/CT for confirming residual disease after SND compared with MRI, CT, or ultrasound fine-needle aspiration biopsy (US-FNA).
Of the entire group, 90% of patients received MRI or CT and 39% received US-FNA as part of the response evaluation three months after chemoradiotherapy. FDG-PET/CT was performed in 38% of patients.
SND was done in 130 patients (14%) due to suspicion of or confirmed residual neck disease by one or more of the imaging methods. Among patients who underwent SND, only 53 (41%) had biopsies that confirmed disease.
According to the analysis, the PPV of FDG-PET/CT for detecting residual disease was 89% compared with 65% for MRI and US-FNA. Moreover, if FDG-PET/CT showed that patients had a complete metabolic response from the treatment, they did not undergo surgery, the authors wrote.
"FDG-PET/CT significantly improved the accuracy of the detection of [pathologic-confirmed residual neck disease], thereby reducing the number of patients undergoing unnecessary SND by 22%," the group wrote.
In addition, the incorporation of FDG-PET into neck surveillance and neck management has long-term cost savings associated with the readmissions, surgical complications, and new surgical interventions needed to treat these complications and rehabilitations after SND, according to the authors.
"The current study demonstrates the superior performance of FDG-PET/CT for response evaluation after chemoradiotherapy in HNSCC and its pivotal role in improving the selection of patients for SND compared with standard diagnostic modalities," the researchers concluded.
The full study is available here.