FDG-PET/CT can help guide therapy in breast cancer, particularly in distant disease staging and treatment response assessment, the leading Austrian researcher Dr. Katja Pinker-Domenig told a hybrid imaging event on 11 November.
"There are also future perspectives with targeted tracers and hybrid imaging with PET/MRI, but we have to be aware of tumor histology," she said at the Conference on Hybrid Imaging Live (CHILI), organized by the European Society for Hybrid, Molecular, and Translational Imaging (ESHIMT).
For T-staging, admittedly, the clinical impact with FDG-PET/CT is limited. "It has a poor sensitivity and specificity compared with dedicated breast imaging," explained Pinker-Domenig, who is a radiologist in the Breast Imaging Service at MSKCC and professor of radiology at Weill Medical College of Cornell University. "The breast primary tumor definitely may not be seen on FDG-PET/CT."
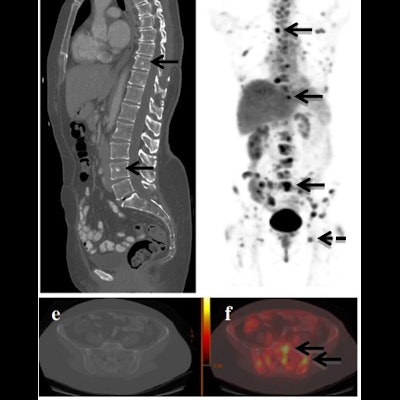
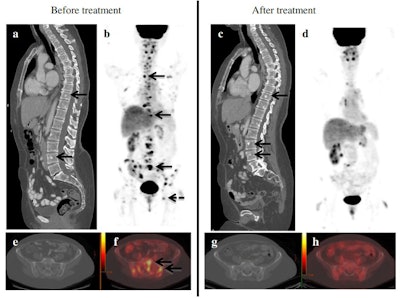 86-year-old woman with metastatic breast cancer before and after first-line endocrine therapy combined with bevacizumab shows stable disease by contrast-enhanced CT and complete response by PET/CT. CT images demonstrate several sclerotic foci in the spine, representing biopsy-proven osseous metastases (arrows in a), with no discernible change after treatment (c). Imaging shows multiple FDG-avid metastases, including the spine (short arrows), pelvis (dashed arrow), and ribs (dotted arrow) (b), with resolution after treatment initiation (d). Axial CT image of the pelvis in the same patient showing no metastases before (e) and after therapy (g). Corresponding axial PET/CT image shows multiple metastases before (f) and resolution of uptake after treatment (h). The patient was still alive at a follow-up of 47 months. Figure courtesy of Drs. Christopher Riedl, Katja Pinker, et al, originally published in EJNMMI.
86-year-old woman with metastatic breast cancer before and after first-line endocrine therapy combined with bevacizumab shows stable disease by contrast-enhanced CT and complete response by PET/CT. CT images demonstrate several sclerotic foci in the spine, representing biopsy-proven osseous metastases (arrows in a), with no discernible change after treatment (c). Imaging shows multiple FDG-avid metastases, including the spine (short arrows), pelvis (dashed arrow), and ribs (dotted arrow) (b), with resolution after treatment initiation (d). Axial CT image of the pelvis in the same patient showing no metastases before (e) and after therapy (g). Corresponding axial PET/CT image shows multiple metastases before (f) and resolution of uptake after treatment (h). The patient was still alive at a follow-up of 47 months. Figure courtesy of Drs. Christopher Riedl, Katja Pinker, et al, originally published in EJNMMI.When it comes to the axillary nodal staging (N-staging), FDG-PET/CT also has relatively poor sensitivity but good specificity when compared with sentinel lymph node biopsy or dedicated axillary breast imaging with ultrasound.
However, FDG-PET/CT is unbeatable for distant staging and N-staging of extra axillary nodes, according to Pinker-Domenig, who is originally from Vienna and also a member of the European Society of Breast Imaging (EUSOBI) Executive Board. She shared the example of a patient with internal chain mammary metastasis.
"This lymph node was prominent on CT and FDG-avid, and was confirmed to be an extra axillary lymph node metastasis, which changed the course of treatment," she told attendees at the virtual meeting.
In the distant staging (M-staging), FDG-PET/CT is superior to any other imaging method, such as CT or bone scan, and it can alter a patient's treatment plan such as primary systemic treatment instead of surgery.
FDG-PET/CT significantly improves the detection of distant metastasis and can change the staging of a patient, she stated. "6% of stage IIA patients, 15% of stage IIB patients, and 28% of stage IIIA patients will be upstaged and thus experience differences in the planned treatment."
Treatment response assessment
FDG-PET/CT can also provide clinical impact in treatment response and is "far superior to other methods when assessing response in patients with distant disease," Pinker-Domenig noted.
"Patients who have metastasis and receive treatment become non-FDG-avid and more sclerotic. With CT alone, we see new sclerotic lesions and it's impossible to know if it's progressive disease, or sclerotic bone metastasis, or treatment effect. This question is easily answered with an FDG-PET/CT scan, where the metastasis is no longer avid and sclerotic but clearly a treatment effect," she said.
In a study comparing FDG-PET/CT with contrast-enhanced CT for prediction of survival in patients with stage IV breast cancer, 43% of the RECIST non-responders were classified as responders with FDG-PET/CT.
"FDG-PET/CT provides significant clinical value accurately classifying responders as such," she said. "With FDG, we expand patient eligibility to other treatments."
Recent research also showed that, when sticking to RECIST alone, a significant portion of patients would not have been able to benefit from novel treatment options.
"With PET/CT we can not only guide treatment decisions but also increase eligibility for patients to have access to novel treatments they can benefit from," Pinker-Domenig told attendees.
FDG-PET/CT is also way superior when identifying recurrent diseases in metastatic patients who have already been treated, she added.
However, radiologists should be aware that FDG-PET/CT also has limitations depending on tumor histology.
The majority of breast cancer cases are invasive ductal carcinomas (IDC). Approximately 15% are invasive lobular carcinomas, which are molecularly different and, on average, less FDG-avid than IDC.
Knowing that the patient has either invasive lobular carcinoma (ILC) or IDC from the beginning is therefore crucial before using FDG, she cautioned.
With the recent inclusion of FDG-PET/CT in the National Comprehensive Cancer Network (NCCN) guidelines as an optional diagnostic method will push its use in clinical practice, Pinker-Domenig believes.
"We're now allowed to perform it. That means insurances will be more inclined to reimburse for those tests. It's a step in the right direction and it will expand access to the examination," she said.
As future directions, she thinks the use of targeted tracers such as fluoroestradiol (FES) and the clinical implementation of PET/MRI. A multiparametric approach with PET/MRI makes a lot of sense to provide an overlap of information, as each modality provides complementary information.
"In this context the one-stop-shop approach is the most relevant. MRI is the modality of choice to initially stage the tumor in the breast. With FDG-PET/CT, we have benefits in distant staging. With FDG-PET/MRI, you can improve the overall diagnostic staging accuracy," she concluded.