After four days of intensive teaching, networking, updating, and discussions of the latest news, the German radiological congress, the DRK, is over. It fulfilled all expectations, and the breast MRI sessions were particularly strong.
There is still great controversy about how breast MRI should be performed in the future and whether it can save money. The congress committee gathered many prominent experts sharing their opinions and visions. One of the topics discussed most controversially is certainly the best indication for breast MRI.
"Usually, people claim breast MRI is an expensive examination," explained Dr. Clemens Kaiser, from the department of clinical radiology at University Hospital Mannheim, who has both an MD qualification and a master's degree in economics, and is the son of Dr. Werner Kaiser, a pioneer in breast MRI.
 "Die weissen Männer," or the white men, entertained DRK attendees at the social get together on the opening day of the congress. Image courtesy of Deutschen Röntgenkongress.
"Die weissen Männer," or the white men, entertained DRK attendees at the social get together on the opening day of the congress. Image courtesy of Deutschen Röntgenkongress.Kaiser investigated whether breast MRI has the potential to even save costs in the management of women with unclear results in the conventional workup. Such patients usually do not receive breast MRI, but are sent to further workup, e.g., biopsy and surgery.
"This costs a lot of money and results are often negative or inconclusive. Breast MRI can be helpful in these patients and I think it is an ideal indication," he said, adding there is a lot to learn and to share and it's important to reach a radiological quality level for the benefits to be realized.
In a cohort of 1,488 patients, he evaluated this indication in a study sponsored by a large German insurance company. The study was conducted between April 2006 and September 2011. Of these patients, 142 were referred to biopsy, 124 because the MR findings detected something suspicious. Eighteen received a biopsy. More than 1,300 patients didn't receive a biopsy, but they were subject to follow-up or the researchers tried to reach the patients by letter to get some information about their health status.
Without breast MRI, all patients would have been sent to biopsy, but the majority of diagnostic problems were solved with MRI and most biopsies were avoided, Kaiser noted. If his group's approach is compared with the conventional algorithm for the workup of suspect breast lesions, there is tremendous potential for breast MRI to save money if "problem-solving" is considered as a potential new indication, he said.
 What's happening today? That was the question asked by delegates from Vienna, Erlangen, and Hamburg, as they studied the RöKo daily newspaper. The program was packed with scientific and educational presentations covering all aspects of general radiology and numerous subspecialties.
What's happening today? That was the question asked by delegates from Vienna, Erlangen, and Hamburg, as they studied the RöKo daily newspaper. The program was packed with scientific and educational presentations covering all aspects of general radiology and numerous subspecialties.Molecular advances
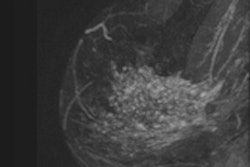
Dr. Pascal Baltzer, from the Medical University of Vienna, gave a fascinating overview of the technical background, clinical reality, and potential future perspectives of molecular breast MR. "We have a wide range of advanced MR techniques at our hands to describe physiologic and pathologic breast tissue in detail," he said.
These techniques include diffusion-weighted and diffusion-tensor imaging, spectroscopy, and dynamic contrast imaging (DCE). The latter provides a functional parameter of tissue vascularization, and certainly forms the basis of every breast MR exam. "In its basic format, you need only a standard temporal resolution. Of course it is technically possible to further increase temporal resolution. The additional clinical value has not been proven, yet the high temporal resolution DCE can be biased by signal noise, real pharmacokinetic analyses are challenging and not likely to improve your diagnostic performance," he noted.
He does not recommend high temporal resolution MRI outside the academic setting, but regards standard DCE is a must in every breast MRI examination. The situation is similar to MR spectroscopy of the breast, a promising technique providing the only in vivo approach to chemically analyze breast tissue. Yet, as clinical radiologists, we need data, Baltzer said.
"At the present time, there is no clear evidence that MR spectroscopy really helps us to solve our diagnostic problems," he added, quoting a meta-analysis he recently published in the June issue of Radiology that showed sensitivity is not likely to be increased by the technique. Furthermore, you need a fairly large mass-like lesion to acquire a high-quality spectrum; such tumors are usually not the diagnostic troublemakers.
The most promising and best evaluated method for molecular breast imaging is diffusion-weighted imaging (DWI). It is fast to acquire and fairly robust, and it gives a more or less quantitative measure of tissue cellularity, and thus an excellent surrogate for malignant tumor growth, Baltzer said. He recommends including DWI into every clinical breast MR protocol.
 After a tough day at the congress, young scientists and medical students attended a special reception for the "brightest minds in radiology" at the Cremon bar. This trendy location gave DRK attendees a chance to relax, network, and exchange the latest news in clinical and academic radiology.
After a tough day at the congress, young scientists and medical students attended a special reception for the "brightest minds in radiology" at the Cremon bar. This trendy location gave DRK attendees a chance to relax, network, and exchange the latest news in clinical and academic radiology.Take a deep breath: The next generation
The organizers of DRK 2013 realize the need to invest in youth and teach the best medical students what a fascinating job every radiologist has. Accordingly, they again provided a program for motivated youngsters. Students selected for the "brightest minds in radiology" scheme received a travel grant and were invited to attend the congress for free. Even more important, special sessions were organized for these potential new colleagues. Such courses were very well attended, and due to the didactic skills of the presenters, they were highly popular. During the sessions, a special student's lounge provided snacks and drinks to relax and network. In addition, a special evening reception in a trendy bar at the legendary Cremon street was organized for delegates.
For young academic radiologists, attending the first congress day was a must. During the two "young investigator award" sessions, almost all areas of radiology were covered in a series of presentations given by Germany's most promising talents. The idea behind it is residents with a special interest in academic radiology present their latest work followed by a short discussion. Then the jury, led by Dr. Fabian Kiessling, head of experimental molecular imaging at the University Hospital Aachen, had the tough job to decide which presentations were the best.
Finally, two papers received awards. One was authored by Dr. Julius Renne and colleagues from the Institute of Radiology at Medical School Hannover. He presented a paper titled "Functional analysis of pulmonary inflammation after bronchial provocation by T1 mapping." Using a standard clinical 1.5-tesla MR system, Renne and colleagues developed a method to noninvasively monitor inflammatory changes in patients with allergic asthma. This work demonstrates the potential of MRI not only as a fascinating scientific instrument, but also as a promising tool in the understanding of pathophysiology processes in pulmonary disease.

 The weather in Hamburg during DRK was fairly mixed. In the foggy and rainy morning, it was easy to attend the congress, but in the afternoon, the wonderful sunny weather arrived. The photos show the main entrance to the Congress Centre Hamburg (CCH), and the Hamburg TV tower.
The weather in Hamburg during DRK was fairly mixed. In the foggy and rainy morning, it was easy to attend the congress, but in the afternoon, the wonderful sunny weather arrived. The photos show the main entrance to the Congress Centre Hamburg (CCH), and the Hamburg TV tower.Certainly it is not possible to give a thorough review of all refresher courses, scientific sessions, and "fit for the specialist" talks. The latter are intended for young radiologists who are preparing for the board certification and were -- as usual -- sold out. Let me therefore highlight two presentations that were of special interest to me:
The "radiological blood test": As radiologists, we do not have any "blood tests," and we do not obtain numbers and quantitative information. This is why our assessment is -- even if we are doing an excellent job -- prone to observer-related bias. Also, this really has a high impact on our report, as the assessment of a colleague might not be comparable to one's own impression. This is particularly challenging in complex techniques such as MRI. Dr. Matthias Benndorf from the University Radiology Clinic, Albert Ludwig University in Freiburg presented an elegant new approach to solve this problem.
In his work on lesion composition, he applied automatic spatial correlation as a potential user-independent quantitative parametric measure to assess tissue heterogeneity. The results were presented at the poster session, and the conclusions are encouraging. Indeed this method could boost the reliability of our radiological report. Not surprisingly, Benndorf received a top award at DRK 2013.
Flat-detector CT: Patient safety and workflow. Dr. Stefan Lang of the department of neuroradiology at the Friedrich Alexander University Erlangen (head: Dr. Arnd Dörfler) presented fresh data on flat-detector CT (FD-CT) in the angio suite. In the daily routine of an interventional neuroradiologist, FD-CT is a new and promising tool. It allows generating a 3D dataset similar to a conventional multislice CT scans. It can be performed during neurointerventional procedures. Accordingly, it is not necessary to move the patient to the (conventional) CT or MRI. This enhances the clinical workflow and certainly is beneficial for the usually very sick patient.
Nevertheless, the diagnostic performance of FD-CT is not fully understood. Accordingly, Dr. Lang evaluated the accuracy of FD-CT for the assessment of intraventricular hemorrhage and hydrocephalus. The results are encouraging, and the method shows excellent performance in most regions. Flat-detector CT is certainly an accurate method with great benefit in workflow and potential impact on patient safety, Lang concluded.
The slogan chosen by the congress committee for the meeting was "Radiology is the future." Dr. Mathias Langer, the medical director and a professor of radiology at the University Radiology Clinic, Albert Ludwig University in Freiburg, was this year's congress president. He elegantly explained this motto: Now in the 21st century, our specialty provides an ever-growing potential to integrate multiple disciplines, offering unique diagnostic and prognostic information both to our fellow colleagues and -- even more important -- to our patients. You do not need prophet-like skills to predict that radiology will develop even further and faster in the next years and decades. This is certainly a tough but wonderful challenge and for this we need highly motivated, excellent trained radiologists, he concluded.
After four days packed with networking, new scientific data, and refreshed knowledge in clinical radiology, there is no doubt that radiology is the future. See you next year!
Dr. Dietzel is a radiologist at the Friedrich-Alexander University Erlangen-Nürnberg, Germany, and a member of AuntMinnieEurope.com's editorial advisory board.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.