It's time to think again about the use of computed radiography (CR) detectors when it comes to spotting breast cancer, U.K. researchers have found. In their study, digital radiography (DR) performed significantly better than CR for identifying calcification clusters and noncalcification lesions.
Mammograms were collected from one screening center in this observer study, led by Dr. Alistair Mackenzie from the National Coordinating Centre for the Physics in Mammography in Guildford, U.K. The images were adapted to simulate four types of detectors at the same radiation dose: DR detectors with amorphous selenium (a-Se) and cesium iodide (CsI) convertors, and CR detectors with a powder image plate (PIP) and a needle image plate (NIP). Seven observers marked suspicious and benign lesions. The researchers found DR detectors pinpointed more cancers than CR, and they published their findings in European Radiology (25 June 2015).
"We have shown significant differences in the detection of lesions between detector types when the same dose was used," Mackenzie and colleagues wrote. "The detector type and its potential effect on cancer detection must be considered during the procurement process for systems. The use and setup of CR imaging systems in mammography should be reconsidered."
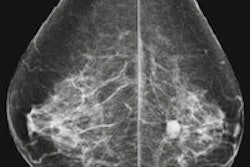
 Example of an inserted calcification cluster converted to appear for the four detector types of the study at the same dose. From left to right: a-Se, CsI, CR NIP, CR PIP. All images courtesy of Dr. Alistair Mackenzie.
Example of an inserted calcification cluster converted to appear for the four detector types of the study at the same dose. From left to right: a-Se, CsI, CR NIP, CR PIP. All images courtesy of Dr. Alistair Mackenzie.How CR stacks up
CR is still in widespread use, particularly in Southern Europe, Mackenzie noted in an email to AuntMinnieEurope.com.
"Despite the current evidence, there is still some strong feeling that there is not a strong relationship between image quality and cancer detection. This work does show that the reduction in cancer detection found by other papers must be largely due to the technology and that the effect is not only for calcification clusters, but all types of cancers," he stated.
Many studies have compared the clinical performance of full-field digital mammography with film-screen mammography, but only a few have compared cancer detection performance with different digital detectors. Two retrospective studies demonstrated the cancer detection rate using PIP CR was lower than with DR systems. To date, no clinical studies have reported on the cancer detection rate using the potentially better NIP CR technology, according to the study authors.
There are many confounding factors when it comes judging different types of imaging detectors including differences in women, radiologists, x-ray equipment, dose, and radiographic practice, making comparison challenging. The researchers took a stab at comparing the detectors in their observer study based on a method to adapt one set of mammograms to appear with the image quality of a range of detectors: DR detectors with a-Se and CsI convertors and also CR detectors with PIP and NIP phosphors.
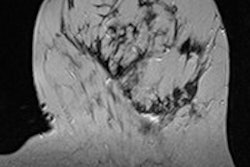
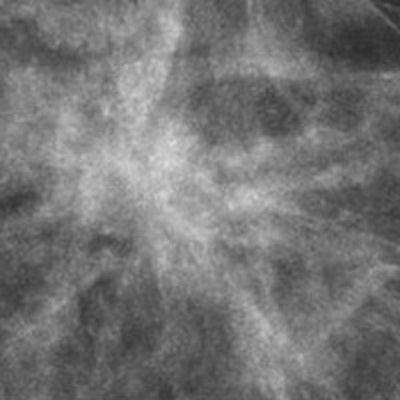
 Example of a real mass (noncalcification lesion) converted to appear for the four detector types of the study at the same dose. Top left: aSe; top right: CsI; bottom left: CR NIP; bottom right: CR PIP.
Example of a real mass (noncalcification lesion) converted to appear for the four detector types of the study at the same dose. Top left: aSe; top right: CsI; bottom left: CR NIP; bottom right: CR PIP.From April 2011 to December 2012, all available mammograms with a malignancy and a random selection of biopsy-proven benign lesions and normals were collected from systems by Hologic to create a database. An expert radiologist, who did not participate in the study, marked a region of interest (ROI) around the cancers and benign lesions in the database and classified their appearance (mass, distortion, focal asymmetry, calcification clusters) and conspicuity (very subtle, subtle, or obvious) in each view.
Then seven observers were recruited from two hospitals. Each observer was an accredited reader working in the National Health Service (NHS) breast screening program with between three and 21 years of experience and reading more than 3,500 screening mammography cases annually. They were asked to mark any suspicious or benign lesions, and the following instruction was applied to each lesion marked: Indicate whether you would recall this patient on the basis of this lesion, along with your confidence in this decision, i.e., your confidence that a recalled lesion will be malignant.
| Comparison of cancer detection fraction (CDF) for CR NIP, CR PIP, and DR |
|||
| DR arm | Difference in CDF of CR NIP & DR | Difference in CDF of CR PIP & DR | |
| Calcification clusters, DR: a-SE | -28% | -45% | |
| Calcification clusters, DR: CsI | -23% | -41% | |
| Average difference in CDF | -26% | -43% | |
| Noncalcification lesions, DR: a-Se | -7% | -8% | |
| Noncalcification lesions, DR: CsI | -13% | -14% | |
| Average difference in CDF | -10% | -11% | |
The maximum estimated differences in cancer detection in screening were 15% and 22% lower for CR NIP and CR PIP, respectively, compared with DR at the same dose, the authors noted.
Limitations
One of the weaknesses of the study was that the radiographic factors were the same for the simulated images as for the original images, which may not be optimal for other detectors.
"The image quality levels used were for well-setup equipment, and so this study does not account for deterioration and artifacts that may occur," the authors wrote. "Ultimately, it must be realized that the study arms are representative of detectors types rather than specific detectors."
Mackenzie and colleagues plans to continue with this published work and examine the correlation between their results and physical measures of image quality, he said.