When transitioning from film-screen mammography (FSM) to full-field digital mammography (FFDM), going digital increases the number of repeated recalls for the same mammographic abnormality, found a large Dutch study published on 14 May in European Radiology.
The research group compared screening outcomes in women recalled twice for the same mammographic lesion before, during, and after the transition from FSM to FFDM, finding more women were repeatedly recalled during and after the transition to FFDM. The cancer risks were comparable before and after the transition, according to lead author Dr. Rob van Bommel from the radiology department at Catharina Hospital in Eindhoven, the Netherlands.
"We found an increased recall rate during the transition from film-screen to digital screening mammography, both for women recalled only once or recalled twice for the same lesion, and these increased recall rates persisted after the transition," he noted.
In addition, the positive predictive value (PPV) of recall for women with a repeated recall for the same lesion was comparable before and after the transition to digital screening. Furthermore, the cancers showed more favorable tumor characteristics than interval cancers.
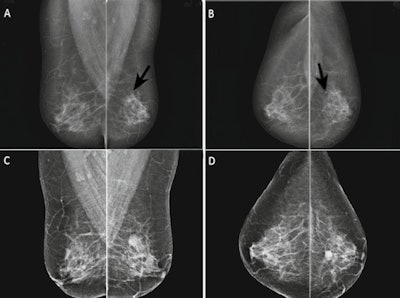 Patient example, repeated recall after previous false-negative recall. Two-view mammogram (A: mediolateral oblique view; B: craniocaudal view) at first recall in 2009 shows a round mass with obscured margins, located dorsally in the left breast (arrows). Ultrasound showed a 4.5-mm mass, interpreted as a simple cyst, and the lesion was classified as BI-RADS 2. Two years later the woman was recalled again because of an increased size of the mass (C, D), and ultrasound now showed a complex cyst of 14 mm. Pathology revealed an invasive ductal carcinoma and intraductal papillary carcinoma without axillary metastasis. Image reprinted with permission from European Radiology.
Patient example, repeated recall after previous false-negative recall. Two-view mammogram (A: mediolateral oblique view; B: craniocaudal view) at first recall in 2009 shows a round mass with obscured margins, located dorsally in the left breast (arrows). Ultrasound showed a 4.5-mm mass, interpreted as a simple cyst, and the lesion was classified as BI-RADS 2. Two years later the woman was recalled again because of an increased size of the mass (C, D), and ultrasound now showed a complex cyst of 14 mm. Pathology revealed an invasive ductal carcinoma and intraductal papillary carcinoma without axillary metastasis. Image reprinted with permission from European Radiology.Transitioning from film to digital
Previous research has shown the transition to full-field digital mammography increased the breast cancer detection rate, especially of low- and intermediate-grade ductal carcinoma in situ (DCIS) and lower-grade invasive cancers. The increased cancer detection rates are usually accompanied by higher recall rates and lower PPV of screening mammography at FFDM than at FSM, the authors explained.
A recent study by Dr. Elisabeth Klompenhouwer published in Breast Cancer Research and Treatment (June 2014, Vol. 145:2, pp. 429-437) found that the first round of FFDM (FSM screen followed by a subsequent FFDM screen) significantly increased the proportion of women recalled twice for the same lesion, with a lower PPV of these lesions. In that study, subsequent FFDM screens were compared with digitized FSM screens. It is assumed fewer women experience a repeated recall for the same lesion after this transition; however, data on this issue are lacking -- until now.
Van Bommel and colleagues sought to determine screening outcomes in women with a repeated recall for the same mammographic abnormality in three screening cohorts (before, during, and after the transition from FSM to FFDM screening mammography) and compared the tumor characteristics in these women with those with interval breast cancers.
Increased rate of repeat recalls
The study was performed in a southern, biennial screening mammography region of the Netherlands. Screening mammograms were obtained at four specialized screening units. The transition from FSM to FFDM screening mammography took place in 2009-2010. A consecutive series of 267,895 subsequent FSM screens with a prior FSM screen (FSM-FSM) were obtained between January 2000 and April 2010.
A total of 91,941 subsequent FFDM screens with a prior previous FSM screen (FFDM-FSM), and 90,407 subsequent FFDM screens with a prior FFDM screen (FFDM-FFDM) were obtained between May 2009 and July 2013.
The researchers included women with a repeated recall for the same mammographic abnormality: 37 at subsequent FSM screening, 54 transitioning from FSM to FFDM, and 65 with a FFDM screen.
| Recall rate, malignancies, and PPV transitioning from FSM to FFDM | |||
| Repeated recalls | Malignancies | PPV | |
| FSM followed by FSM | 1.2% (37/3,217) | 13 | 35.1% |
| FSM to FFDM transition | 2.2% (54/2,494) | 13 | 14.8% |
| FFDM followed by FFDM | 2.8% (65/2,360) | 16 | 24.6% |
More women experienced a repeated recall for the same mammographic lesion during the transition from FSM to FFDM screening, and the phenomenon persisted after the transition, the study authors wrote. The increased chance of a repeated recall came along with a nonsignificantly decreased PPV of recall. Also, cancers diagnosed after a repeated recall showed a more favorable tumor stage and grading than interval cancers.
In terms of how the tumors compared with interval cancers, invasive cancers at repeated recall were smaller than interval cancers with less lymph node involvement, according to the researchers.
"To our knowledge, this is the first study that compares the proportions of women recalled twice for the same mammographic abnormality before, during, and after the transition from film-screen to digital screening mammography," they explained.
Limitations
Extrapolation of van Bommel's results to other screening programs may be limited as the study designs of other programs vary considerably. For instance, the Dutch screening program is characterized by a lower referral rate than most European and U.S. screening programs. Moreover, screening outcome parameters will be influenced by the screening interval used at screening programs such as biennially or screening every three years.
Also, mammographic screening in the Dutch program is performed in a standardized fashion by certified screening radiographers and screening radiologists, who frequently receive feedback on their individual performance.
In addition, Dutch breast units show variations in the quality of diagnostic imaging and clinical assessment, which may influence the accuracy of recall outcome.