An audit on preimaging relocation in patients with low-velocity shoulder dislocations and the efficacy of clinicians in identifying and documenting underlying pathology has shown that it may be a safe, appropriate option for patients with recurrent dislocations.
The study was presented by Dr. Graeme Abreu from the Department of Medical Imaging at Royal Brisbane and Women’s Hospital at the annual scientific meeting of the Royal Australasian and New Zealand College of Radiology (RANZCR 2025).
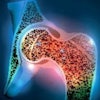
 Dysplastic glenoid tubercle predisposing patient to recurrent dislocations.All figures courtesy of Dr. Graeme Abreu, Royal Brisbane and Women’s Hospital, and presented at RANZCR 2025 ASM.
Dysplastic glenoid tubercle predisposing patient to recurrent dislocations.All figures courtesy of Dr. Graeme Abreu, Royal Brisbane and Women’s Hospital, and presented at RANZCR 2025 ASM.
Patients presenting with recurring low-velocity shoulder dislocations were less likely to have acute underlying pathologies. Such patients are often younger and more active, Abreu explained, with increased joint instability following each dislocation -- and therefore more frequent recurrent dislocations. Lifetime radiation exposure is a concern with this patient group, given the recurrence.
The author writes that shoulder dislocations are very common in emergency departments, comprising 50% of the total of major joint dislocations presenting, with more than 95% being anterior dislocations.
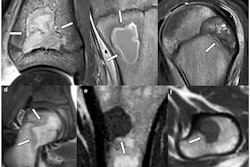
 Greater tuberosity fracture overlooked on initial imaging.
Greater tuberosity fracture overlooked on initial imaging.
Abreu performed a retrospective review of patients presenting with shoulder dislocation as the diagnosis or in triage notes between July 2023 and February 2024. All patients included in the review had received imaging. Records and imaging were reviewed for pre- and post-relocation imaging pathology, along with concordance between the findings of the treating clinician with those of the radiologist, as well as postdischarge follow-up recommendations or referrals.
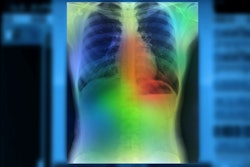
 Acromioclavicular dislocation in suspected shoulder dislocation.
Acromioclavicular dislocation in suspected shoulder dislocation.
In total, radiographic pathology was reported on 32% of pre-relocation images and 46% of post-relocation images. Furthermore, 95% of fractures reported by clinicians were confirmed by radiology. However, between 40% and 44% of patients noted as having no fracture present were subsequently determined by radiology to have a fracture.
“Lesion identification was also demonstrated to be more accurate on post-relocation imaging,” the author pointed out.
Nevertheless, Abreu added that despite the discrepancies in the identification of fractures, postpresentation follow-up and referral were appropriate in more than 95% of all the cases of suspected shoulder dislocation.
Furthermore, the findings show that patients with recurrent, low-velocity dislocations were unlikely to have an unexpected underlying pathology, which would indicate “a level of safety in pre-imaging relocation within this population, thus minimizing total lifetime radiation exposure and potential stochastic effects, reducing length of patient discomfort prior to relocation and shorter length of emergency department admission times thus improving departmental patient flow.”
Read the full RANZCR 2025 poster here.