Researchers from the Beaumont Hospital in Dublin have asserted that patients under the age of 45 who present to the symptomatic clinic with a normal breast exam should not undergo imaging, but the group recommends all women with a normal clinical exam should receive a risk assessment.
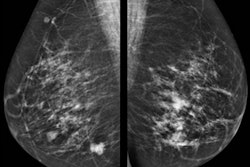
The team assessed the value of mammography in symptomatic patients with normal breast exams. During the eight-year study period, 12,426 specialist breast clinic visits (11,530 consecutive patients) were included, 81% of whom had subsequent diagnostic breast imaging.
 The 820-bed Beaumont Hospital is a large teaching hospital founded in 1987. It is managed by RCSI Hospitals, one of the hospital groups established by the Health Service Executive. Courtesy of Noel Bennett / Alamy Stock Photo.
The 820-bed Beaumont Hospital is a large teaching hospital founded in 1987. It is managed by RCSI Hospitals, one of the hospital groups established by the Health Service Executive. Courtesy of Noel Bennett / Alamy Stock Photo.These five clinical questions were addressed:
- How frequently are patients with normal breast exams undergoing imaging?
- What is the diagnostic yield of this imaging?
- What clinical factors impact diagnostic yield?
- Do the benefits of imaging outweigh the harms in the study population, or in a subset?
- Is this a cost-effective use of healthcare resources?
"The primary study aim is to provide clinicians with an evidence-based decision-making tool for assessing a symptomatic patient's need for breast imaging in the setting of a normal breast exam, and ultimately avoid unnecessary imaging," the authors noted.
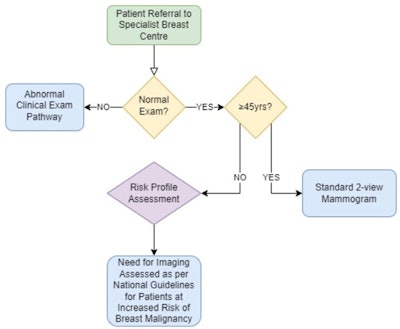 Clinical decision-making tool proposed by Beaumont research group. All remaining figures courtesy of M.R. Common et al, presented at ECR 2023.
Clinical decision-making tool proposed by Beaumont research group. All remaining figures courtesy of M.R. Common et al, presented at ECR 2023.Study logistics
The retrospective observational study was conducted at Beaumont Breast Centre, Beaumont Hospital. Consecutive new referrals attending the symptomatic breast clinic from 1 January 2014 to 31 December 2021 were included.
Patients with a previous diagnosis of breast cancer, patients attending for surveillance (not first visit) due to an established high-risk profile, and patients followed for over a year with serial breast imaging after initial clinic visit without repeat clinical exam were all excluded.
Biopsies were performed in 713 patients, and they yielded 554 benign (B1/2), 72 indeterminate (B3/4), and 87 malignant diagnoses. Five patients with malignant biopsies and six patients with indeterminate biopsies were managed nonsurgically. A total of 148 patients underwent definitive resection, yielding 91 confirmed malignancies. Overall, the incidence of breast cancer was 7.7 per 1,000, and 9.5 per 1,000 in those imaged.
"Follow-up data for patients who did not receive imaging was unavailable at the time of analysis. Consequently, the difference in breast cancer incidence between the imaged and un-imaged populations cannot be fully explained, but likely represents a combination of undiagnosed cancers and overdiagnosis," the team reported in an e-poster presentation at ECR 2023.
As age increases, the incidence of malignancy rose, while the negative biopsy rate decreased, they added. "Consequently, the benefit-to-harm ratio of breast imaging increases as population age increases."
Within the 50- to 70-year-old age group, a statistically significant difference in incidence exists, indicating that a symptomatic patient presenting to a specialist breast clinic is more likely to have cancer than the age-matched asymptomatic patient undergoing screening. Whether or not this difference persists in patients under 50 is difficult to determine, as there is no direct means of population comparison.
Also, there was a statistically significant tripling of the odds ratio and doubling of breast cancer incidence in imaged patients ages 40 to 45 versus 45 to 50, according to the authors.
| Estimated costs relating to breast clinic assessment | |
| Investigation | Cost in euros |
| Consultation and clinical exam | 72.57 |
| Mammography | 91.97 |
| Ultrasound | 115.23 |
| Ultrasound-guided fine-needle aspiration/aspiration | 288.62 |
Economic analysis was conducted to evaluate cost of examination, imaging, and biopsy in each age band. There was a significant difference in investment efficiency between the 40- to 45-year-old and 45- to 50-year-old age groups. The number of patients imaged and costs to diagnose one cancer are both reduced by roughly 61% in the higher age bracket -- the largest difference between any two adjacent brackets, they noted.
If a minimum imaging age of 45 is selected from the table below, significant improvements in imaging required per cancer (254 vs. 85, 67% reduction) and cost per diagnosis are seen (67,833 euros vs. 22,929 euros, 66% reduction). As a result, 4,232 imaging slots would be freed, 309 unnecessary biopsies avoided, and 1.2 million euros saved at the cost of 17 undiagnosed cancers in 10,067 imaged patients, the researchers pointed out.
| Age-limited cost analysis | |||||||||
| Age limit | Count | Imaging | ≥R3 | Biopsy | Negative biopsy | Cancer | Image/cancer | Total cost | Cost/cancer |
| Younger than than 40 | 2,643 | 2,121 (80.25%) | 123 | 144 | 95.14% | 7 | 303 | 564,806.87 | 80,686.70 |
| Younger than than 45 | 5,322 | 4,323 (81.23%) | 270 | 309 | 94.5% | 17 | 254.29 | 1,153,169.18 | 67,833.48 |
| Younger than than 50 | 7,693 | 6,281 (81.65%) | 411 | 469 | 91.47% | 40 | 157.03 | 1,680,546.71 | 42,013.67 |
| Younger than than 70 | 11,285 | 9,122 (80.83%) | 561 | 649 | 89.06% | 71 | 128.48 | 2,435,425.23 | 34,301.76 |
| Younger than than 100 | 12,426 | 10,067 (81.02%) | 615 | 713 | 86.54% | 96 | 104.86 | 2,684,279.53 | 27,961.25 |
A more conservative minimum imaging age of 40 compared with the 40- to 45-year-old age range shows more modest improvements in imaging required per cancer (303 vs 254, 16% reduction) and cost per diagnosis (80,687 euros vs. 58,836 euros, 27% reduction). As a result, 2,121 imaging slots would be freed, 144 unnecessary biopsies avoided, and 564,806.87 euros saved at the cost of seven undiagnosed cancers in 10,067 imaged patients, they continued.
Hypothetical implementation of the clinical decision-making tool proposed by the Beaumont team over the eight-year study period would have led to a minimum of 4,323 imaging slots freed (540/year), avoidance of 309 unnecessary biopsies (39/year), and 1.2 million euros saved (144,146 euros/year) -- at the expense of 17 undiagnosed cancers (2.13/year).
The authors hope these results will provide an evidence-based approach to assessing patients' needs for breast imaging, given a normal breast exam, and empower clinicians to educate symptomatic patients about the benefits and risks of breast imaging.
To view the whole ECR 2023 e-poster, go to the EPOS section of the congress organizers' website. The co-authors of the ECR e-poster were P. Rohan, E. Downey, N. Hambly, N. Ní Mhuircheartaigh, J. Kerr, C. Power, A. D. Hill, D. Duke.