Digital breast tomosynthesis (DBT) plus synthesized mammography can detect more invasive breast cancers in dense breasts than digital mammography alone, a German study of nearly 100,000 women published in Radiology found.
Using data from the TOmosynthesis plus SYnthesized MAmmography (TOSYMA) trial, a team led by Dr. Stefanie Weigel from University of Münster wrote that this finding is applicable to all breast density categories apart from women with predominantly fatty parenchyma.
"The results demonstrate that DBT contributes to an increase in early diagnosis of breast cancer, probably by reducing radiological superposition and masking effects, and so it can reduce limitations of digital mammography," Weigel told AuntMinnie.com.
It's well known in the breast imaging community that dense breasts are mammography's kryptonite. Previous research shows that in women with dense breasts, standard digital mammography has low breast cancer detection rates. This also means higher interval cancer rates with poorer prognosis for women with extremely dense breast parenchyma, as well as lower screening sensitivity.
DBT has shown promise in breast imaging over the past decade since it first became commercialized. The technology is also believed to be better able to help radiologists analyze dense breast tissue.
Weigel and colleagues previously explored data from the TOSYMA trial that showed that the combined approach of DBT plus synthesized mammography had a 48% higher cancer detection rate than full-field digital mammography when it came to routine screening.
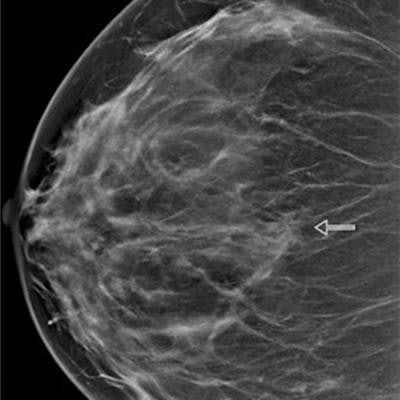
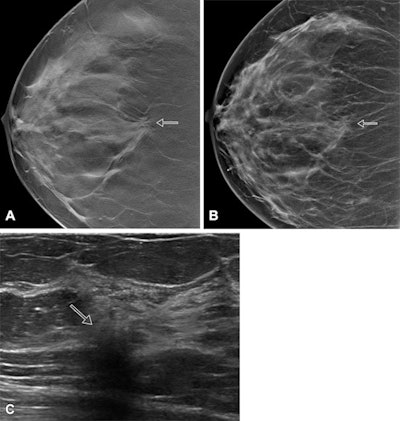 Images show screen-detected invasive breast cancer in dense breast tissue in a 65-year-old woman. The histology was invasive carcinoma of no special type with a tumor size of 10 mm, grade 2. (A) A single section of a DBT scan of the craniocaudal view of the right breast shows a cancer-related spiculated mass with highly suspicious radiologic features (arrow). (B) Corresponding synthesized mammogram of the right craniocaudal view shows that the cancer-related spiculation is less obvious in comparison to the single section (arrow). (C) Correlating ultrasound scan shows the invasive breast cancer as an irregular, indistinct, not parallel, hypoechoic mass (arrow) with a hyperechoic distortion of the adjacent parenchyma. Images courtesy of RSNA.
Images show screen-detected invasive breast cancer in dense breast tissue in a 65-year-old woman. The histology was invasive carcinoma of no special type with a tumor size of 10 mm, grade 2. (A) A single section of a DBT scan of the craniocaudal view of the right breast shows a cancer-related spiculated mass with highly suspicious radiologic features (arrow). (B) Corresponding synthesized mammogram of the right craniocaudal view shows that the cancer-related spiculation is less obvious in comparison to the single section (arrow). (C) Correlating ultrasound scan shows the invasive breast cancer as an irregular, indistinct, not parallel, hypoechoic mass (arrow) with a hyperechoic distortion of the adjacent parenchyma. Images courtesy of RSNA.However, in this most recent study, the team wanted to focus on comparing the invasive breast cancer detection rate of the combined approach versus digital mammography for women with different breast density categories.
The researchers looked at data from a total of 99,558 women with an average age of 57 years. The women were placed into two groups, one for DBT plus synthesized mammography (n = 49,762) and the other for digital mammography (49,796).
The researchers used breast density categories defined by the American College of Radiology's (ACR) BI-RADS, fifth edition. The categories include the following: almost entirely fatty (category A), scattered areas of fibroglandular density (category B), heterogeneously dense (category C), extremely dense (category D).
| Cancer detection rate for DBT + synthesized mammography versus digital mammography (cancers per 1,000 women) | ||
| Tissue type | Digital mammography | DBT + synthesized mammography |
| Entirely fatty tissue | 3.6 | 2.7 |
| Scattered areas of fibroglandular density | 4.3 | 6.9 |
| Heterogeneously dense | 6.1 | 8.3 |
| Extremely dense | 2.3 | 8.1 |
Weigel said the team was surprised by the "substantial magnitude" of the higher detection rates seen in the combined approach arm.
The group noted that the combined approach detected over 3.5 times more cancers than digital mammography alone (odds ratio, 3.8).
"Previous arguments had emphasized limitations of DBT in extremely dense parenchyma, supposedly due to a low-fat proportion and putatively related discrimination problems," Weigel said.
Also, invasive cancers detected with DBT plus synthesized mammography were most often grade 2 tumors. For heterogeneously dense tissue, it was 58% (91 of 156 invasive cancers), while for extremely dense tissue, it was 47% (15 of 32 invasive cancers).
The researchers noted that the frequency with which women with extremely dense breasts presented were similar in both study arms, less than 10%.
The team suggested that based on their results, digital mammography alone is enough for women with breasts in category A, entirely fatty tissue. However, all other categories favor the use of DBT plus synthesized mammography.
Weigel told AuntMinnie.com that the team wants to next evaluate interval cancer rates and advanced breast cancer stages up to the next screening round to "more accurately" explore the long-term benefit of a screening program with DBT.
"We expect data from the cancer registries in 2024 or 2025," she said.
In an accompanying editorial, Dr. Cindy Lee and Dr. Linda Moy from New York University wrote that the study's results highlight the need for "more robust evidence" on the long-term clinical outcomes of DBT screening.
They noted that the TOSYMA-2 endpoints obtained from the prospective follow-up phase, including 12-month and 24-month invasive interval cancer rates, will indicate whether increased invasive cancer detection at screening translates into lower interval cancer incidence.
"With the invasive cancer detection rate representing a surrogate end point for mortality data, results from TOSYMA point toward positive effects of DBT on long-term screening benefits," they wrote. "However, increased screen detection of small cancers without a reduction in interval cancers in the subsequent two-year follow-up would raise questions about possible overdiagnosis."