Less than half of radiologists use guidelines from the European Society of Urogenital Radiology (ESUR) on female pelvic MRI, highlighting the need for an awareness campaign, a survey of European Society of Radiology (ESR) members has found.
"Radiologists worldwide perform female pelvic MRI studies with a technique and indications that are generally in line with the recommendations of the ESUR, (but) barriers and opportunities to improve the knowledge of and adherence to guidelines warrant consideration," noted first author Dr. Stephanie Nougaret, PhD, a radiologist from the Montpellier Cancer Institute, INSERM, University of Montpellier, France, and colleagues.
The authors published their findings on 28 March in Insights into Imaging. Their survey was prompted by wide regional variations in the indications for MRI of female pelvis due to clinical preferences, as well as the limited availability of MRI and potential reimbursement challenges. Also, considerable differences exist in MR image acquisition and interpretation, they explained.
The group's aim was to gather data on current female pelvic MRI practice, patterns of pelvic MRI requests, and MRI protocols, as well as to determine how widely the ESUR guidelines had been implemented in routine clinical practice among ESR members.
The survey opened online on 7 May 2019, and it remained active for five weeks. Among the 5,900 ESR members invited to take the survey, there were 840 respondents (14.2%). The European countries with the higher response rates were Spain and the U.K. (n = 34), Romania (n = 30), and Portugal (n = 20). Outside of Europe, the most responses came from India (n = 85), Saudi Arabia (n=32), and Pakistan (n = 31).
About 51% of survey participants worked in an academic setting, and nearly 60% were women and a third subspecialized in gynecologic imaging, the researchers stated.
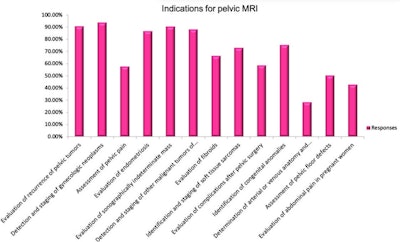
The most common indications for MRI were detection and staging of gynecologic neoplasms (81%), followed by evaluation of suspected or confirmed recurrent pelvic tumor (78%) and sonographically indeterminate adnexal mass (78%).
MRI protocols
Around 94% of ESR members performed MRI exams on a 1.5 and/or 3-tesla machine. Most radiologists used a tailored protocol, as recommended by the ESUR, and 70% of the sample used T2/T1 sequences covering the para-aortic regions.
Oblique sequences perpendicular to the short axis of the uterine corpus or cervix for endometrial and cervical cancer staging were performed by 85% of respondents, and 64% used a slice thickness of 4 mm or higher for axial or axial oblique sequences.
The use of gadolinium-enhanced T1-weighted fast-spin sequences deviated from the guidelines, according to the authors. Only 63.5% of radiologists used contrast-enhanced MRI for the assessment of sonographically indeterminate adnexal masses, and only 40% for evaluation of myometrial masses. Dynamic contrast-enhanced (DCE) MRI was used even less. For example, only 29% of radiologists used DCE-MRI in the assessment of a sonographically indeterminate adnexal mass.
Diffusion-weighted imaging (DWI) was obtained in 41% of female pelvic MRI exams, indicating wider adoption compared with DCE MRI. When DWI images were acquired, the axial plane was used most often and a high b value of 800 or greater was obtained by 64% of radiologists.
Use of reporting guidelines
Questions about reporting were not answered by 233 participants. Of 607 respondents, the standardized report was used by 46% of the 607 respondents. Nearly half of the responders were aware of ESUR guidelines for imaging of the female pelvis (47%). Among them, the reporting guidelines for the staging of endometrial and cervical cancer were the most used.
"Emphasis must be put on developing a universally usable and accepted terminology (lexicon) for these reports," stated Nougaret and colleagues. "For ovarian mass characterization, such a lexicon has recently been published, but further effort is needed."
The use of ESUR guidelines was significantly more frequent among specialists versus nonspecialists (63.5% vs. 39%). The use of DWI, contrast-enhanced imaging and DCE-MRI was significantly more frequent among subspecialized than among general radiologists.
Also, the use of ESUR guidelines was much higher among European (63%) compared with non-European radiologists (35%), but the use of a reporting template was more frequent in non-European (58%) compared with European centers (32%).
The use of ESUR guidelines was more likely among senior radiologists (51%) compared with less experienced radiologists (40%). The use of an oblique plane perpendicular to the long axis of the uterus or cervix, DWI, contrast-enhanced imaging, and DCE MRI were significantly more frequent among senior radiologists compared with junior radiologists.
Other developments
To address the awareness issue, the ESUR produced the Quick Guide to Female Pelvis Imaging. This free 80-page booklet is designed to be used as a raid reference tool to assist in planning the imaging of patients with suspected or confirmed gynecologic disease.
Since the ESR survey was carried out, the ESUR has published other guidelines, such as those related to MRI of cervical and vulval cancer, Nougaret told AuntMinnieEurope.com.
"Fellowship training, including a curriculum dedicated to MRI gynecological evaluation, is another possible benchmark that could clearly improve imaging reporting accuracy," she noted, adding that follow-up surveys are being planned, particularly in the area of O-RADS classification.
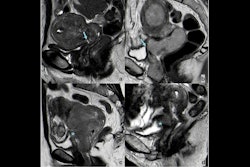
Editor's Note: The image used to introduce this article on our homepage is an MRI scan obtained during straining and evacuation. A large anterior rectocele develops, associated with descent of the posterior pelvic floor. Courtesy of Dr. Francesca Maccioni, Sapienza University of Rome.