Clinicians looking to accurately classify suspicious lymph nodes in prostate cancer patients could have another effective noninvasive option with a unique contrast-enhanced MR imaging technique, according to a study published online on 30 January in the Journal of Nuclear Medicine.
In a direct comparison with gallium-68 (Ga-68) prostate-specific membrane antigen (PSMA) PET/CT, MR imaging with a ferumoxtran-10 nanoparticle contrast agent (nano-MRI) identified significantly more suspected serious lymph nodes, as well as nodes that were significantly smaller. At the same time, the two approaches were fairly complementary, as they both discovered some lymph nodes the other modality missed.
"Although there is no reference standard in this study, the main results mentioned above provide insight into the complementary performance of both modalities by identifying aspects where they agree and disagree," wrote the authors led by Dr. Melline Schilham from Radboud University Medical Centre, Nijmegen, the Netherlands. "Such results allow the definition of future areas of research that need to be addressed in order to define the optimal imaging strategy for prostate cancer patients."
The most effective way to determine the potential health danger of lymph nodes in prostate cancer cases is through dissection. Given that dissection is an invasive procedure that can put a patient at risk for other adverse conditions, there is the "demand and increasing role for noninvasive imaging techniques to detect lymph node metastases in prostate cancer patients," Schilham and colleagues wrote.
Ga-68 PSMA PET/CT has been touted in a number of studies for its prowess in accurately determining the extent of prostate cancer and directing patients to the most appropriate treatments. In addition, nano-MRI, also known as MR lymphography, has garnered attention with its use of ferumoxtran-10 (Ferrotran, SPL Medical) to differentiate between malignant metastatic lymph nodes and benign abnormalities. One study found that nano-MRI with the ultra-small iron oxide particle contrast agent achieved sensitivity of 82% and specificity of 93%.
"Since both modalities rely on different technical and biological features, it was hypothesized that a combined use could even improve lymph node detection," the authors wrote.
So, they set out to explore the "feasibility of a potential complementary role for those imaging modalities by comparing their results in the same patient[s] and identifying differences and similarities in detected lymph node characteristics, irrespective of a reference standard."
This retrospective study looked at 45 patients (mean age, 64 years; range 48-82 years) with either primary prostate cancer (8 patients, 18%) or recurrence (36 patients, 82%). Within a three-week period, all of the subjects underwent Ga-68 PSMA PET/CT (Biograph mCT, Siemens Healthineers) with a tracer dose of 2 MBq/kg body weight and 3-tesla MRI scans (Magnetom Skyra or Trio, Siemens) with ferumoxtran-10 doses based on 2.6 mg/kg body weight and administered 24 to 36 hours prior to the MRI. The combined results revealed a total of 179 suspected lymph nodes in 33 patients, with at least three or more lymph nodes per patient.
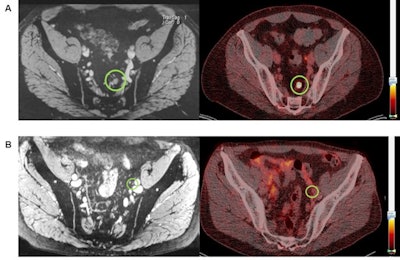 One set of images (A) shows a 7-mm diameter lymph node that is positive on both nano-MRI and PSMA-PET/CT in a patient's left pararectal region. For comparison, the other set of images (B) shows a 4-mm diameter lymph node diagnosed as positive on nano-MRI (left) but negative on PSMA-PET/CT (right) with no Ga-68 PSMA tracer uptake in the region (green circle). Images courtesy of the Journal of Nuclear Medicine.
One set of images (A) shows a 7-mm diameter lymph node that is positive on both nano-MRI and PSMA-PET/CT in a patient's left pararectal region. For comparison, the other set of images (B) shows a 4-mm diameter lymph node diagnosed as positive on nano-MRI (left) but negative on PSMA-PET/CT (right) with no Ga-68 PSMA tracer uptake in the region (green circle). Images courtesy of the Journal of Nuclear Medicine.Nano-MRI was significantly superior by detecting 160 suspicious lymph nodes (89%) in all 33 patients (100%), compared with 71 suspicious lymph nodes (40%) discovered by PSMA PET/CT in 27 patients (82%) (p < 0.001). Of all 160 suspicious lymph nodes, nano-MRI exclusively discovered 108 of them (60%), while PSMA PET/CT was the sole identifier of 19 (11%) suspicious lymph nodes and both modalities similarly spotted 52 (29%) suspicious abnormalities.
In addition, nano-MRI found significantly smaller suspicious lymph nodes (mean size, 5.2 mm; range, 2-16 mm), compared with Ga-68 PSMA PET/CT (mean size, 6 mm; range, 3-16 mm) (p = 0.006).
The fact that both modalities found suspicious lymph nodes the other imaging technique missed suggests "a potential complemental role for nano-MRI to PSMA-PET/CT," Schilham and colleagues added. "However, since the clinical implications of the different results are not well established yet, further investigation in this complementary use is encouraged."



















