
Radiologists from the hospital that carried out the first lung transplant in France on a COVID-19 patient have shared their experiences and knowledge of how imaging can help to improve outcome and minimize the risk of rejection of the transplanted organ.
"Recognition of early signs of rejection is crucial, for better understanding of physiopathologic pathways and optimal management of patients," noted Dr. Ophélie Dana, Prof. Philippe Grenier, and colleagues from Hôpital Foch in Suresnes, France.
If chronic lung allograft dysfunction (CLAD) remains a clinical diagnosis based on spirometry, CT scanning plays an important role in the diagnosis and follow-up of patients to exclude identifiable causes of functional decline when CLAD is first suspected. CT can also detect early abnormalities that can precede the diagnosis of CLAD (particularly restrictive allograft syndrome, RAS) and detect exacerbations and evolution from one phenotype to the other, they explained.
 Hôpital Foch is a teaching hospital affiliated to Versailles Saint-Quentin-en-Yvelines University. Photo courtesy of Hôpital Foch.
Hôpital Foch is a teaching hospital affiliated to Versailles Saint-Quentin-en-Yvelines University. Photo courtesy of Hôpital Foch.The first experimental lung transplants were performed in 1947 by the Russian surgeon Vladimir Demikhov, after which Italian, French, and U.S groups studied lung transplantation. The first clinical lung transplant was performed by Dr. James D. Hardy in Jackson, Mississippi, in 1963. By 1983, 45 lung transplants had been carried out at various centers, and only one patient transplanted in Ghent, Belgium, in 1968 had survived for 10 months, whereas all other patients survived less than a few days.
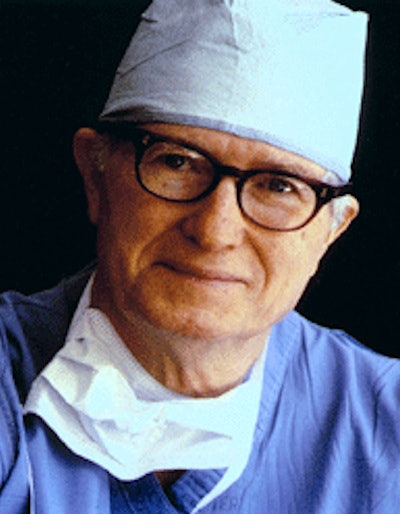 Dr. James D. Hardy, who died in 2003. Photo courtesy of University of Mississippi.
Dr. James D. Hardy, who died in 2003. Photo courtesy of University of Mississippi.Today, over 4,000 lung transplantations are performed per year worldwide, but this remains a challenging area, and long-term outcomes are still poor compared with those of other types of solid organ transplantation, according to Dana and colleagues. The main limitation is chronic rejection, and chronic lung rejection remains one of the major causes of morbidity and mortality after lung transplantation.
"CLAD affects up to 50% of the patients at five years post transplantation and is responsible for reduced survival and reduced quality of life," they stated in an RSNA 2020 e-poster that received a certificate of merit award from the judges. "Multiple phenotypes of lung rejection exist. The term CLAD has been proposed to describe the different processes that lead to a significant and persistent deterioration in lung function without identifiable causes."
What to know about CLAD
CLAD is defined as the substantial and persistent decline in measured forced expiratory volume in one second (FEV1) that is greater than or equal to 20% compared with the baseline value and cannot be explained by other conditions. The baseline value is defined as the mean of the two best postoperative values at least three weeks apart, the authors continued.
The clinical diagnosis of CLAD relies mostly on pulmonary function tests, and it can present as a predominantly obstructive pattern (bronchiolitis obliterans syndrome, BOS), a restrictive pattern (RAS), or a mixed obstructive and restrictive pattern.
"CT plays an important role in the detection and characterization of CLAD and the exclusion of other causes of functional alteration in lung transplants," they added.
The following may be responsible for loss of lung function -- stable and chronic -- where a "new baseline" FEV1 should be defined: decreasing lung function due to the normal aging process; parenchymal or chest wall surgery, phrenic nerve damage; airway or vascular stenosis, chronic pleural effusion, persistent pulmonary edema; post-infective or post-operative chronic scarring; donor/recipient mismatch; and disease recurrence on the allograft.
Potentially reversible functional decline may be due to infection, acute cellular/antibody-mediated rejection, aspiration/gastro-esophageal reflux, and azithromycin reversible allograft dysfunction.
Optimum use of CT
Dana and colleagues recommend an initial CT scan in all patients six months after lung transplantation, when spirometry is expected to be optimal. It should be performed without iodine contrast, in high-resolution (maximum width of 3 mm sections), and at full inspiration and expiration.
Repeat CT studies should be performed when a first drop in FEV1 of more than 10% is seen (possible CLAD), to try to identify an obvious cause, such as infection, drug toxicity, acute rejection, and malignancy. They should also be carried out at the onset of confirmed CLAD and in other cases, depending on the clinical and functional evolution and keeping in mind the possible evolution to a mixed phenotype.
BOS and RAS are both associated with particular CT features, and these entities can be associated (mixed pattern), most of the time with an initial obstructive phenotype developing restrictive features. CT can also play a key role in the identification of many conditions responsible for functional decline, and not related to CLAD, they noted.
First transplant on COVID-19 patient
In November 2020, staff in Hôpital Foch's thoracic surgery department performed the first lung transplant in France on a man who presented with acute respiratory failure due to COVID-19.
 The recovery of a lung transplant patient is often long and sometimes difficult. Image courtesy of Hôpital Foch.
The recovery of a lung transplant patient is often long and sometimes difficult. Image courtesy of Hôpital Foch.This patient, initially treated in the intensive care unit at Lille University Hospital, had developed an extremely serious form of respiratory disease responsible for almost complete destruction of both his lungs, according to a statement issued by the hospital.
His condition showed no signs of improvement, making a lung transplant necessary.
"The choice to use this ultimate and exceptional therapy is not simple and is subject to the results of numerous complementary examinations. The aim is to detect potential contraindications that could cause the failure of this procedure," said Dr. Edouard Sage, the surgeon who is responsible for the lung transplant program at Hôpital Foch.
The procedure went well, the statement reported. "However, we must remain cautious, because the recovery of a lung transplant patient is often long and sometimes difficult," Sage said.



















