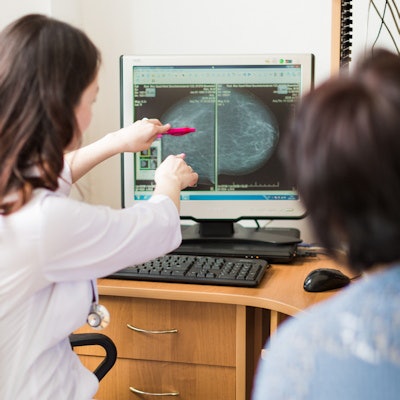
Researchers identified six psychological and socioeconomic factors that influence whether a woman is more or less likely to undergo regular screening mammography. The Turkish research team published their findings on 2 January in Perspectives in Psychiatric Care.
Breast cancer cases are growing in Turkey and other low- and middle-income countries, prompting researchers to look for factors that may influence whether a woman decides to participate in screening activities such as mammography or clinical breast examinations.
The new study, led by Seçil Taylan, PhD, included 1,150 women diagnosed with breast cancer who were registered at a health center in the southern region of the country. Taylan and colleagues asked the women 14 questions about their socioeconomic background and lifestyle factors.
They found statistically significant relationships between six factors and routine mammography screening.
1. Education
Women with higher levels of education reported undergoing biannual mammography more often than those who were less educated. A total of 44% of university-educated women said they received routine mammography compared with 6% of women without a primary school education.
2. Occupation
Occupation also played a role in whether women were likely to undergo mammography. On the high end, nearly 47% of public employees said they underwent biannual mammography, followed by 28% of women who identified themselves as workers or retired, respectively.
In contrast, only 9% of women who identified themselves as housewives said they received a mammogram every two years. Farmers fell in the middle of the other groups, with 18% of women who said they were farmers saying they underwent regular mammography.
3. Health insurance status
Women with health insurance were much more likely to engage in routine mammography than those without access to social health insurance. Nearly 18% of women with health insurance underwent regular mammography, compared with just 1% of women without insurance.
Health insurance status was one of the largest predictors of whether a woman underwent routine mammography in a secondary analysis conducted by the researchers to determine the factors that had the greatest influence on screening. In that analysis, women had 6.3-times greater odds of undergoing mammography if they had social health insurance.
4. Family history of breast cancer
A greater proportion of women with a family history of breast cancer said they underwent regular mammography than those without a family history of breast cancer. That relationship also varied by whether the familial breast cancer occurred in a first- or second-degree relative.
A total of 48% of women with a mother or sister with breast cancer said they underwent biannual mammography, as did 37% of women with an aunt or grandmother with breast cancer. In comparison, 13% of women without a family history of breast cancer reported undergoing regular mammography.
5. Perceived breast cancer risk
Women who thought they had a higher risk of developing breast cancer in the next 10 years were more likely to undergo mammography. About 37% of women who thought they had a high risk of breast cancer reported undergoing mammography every two years, followed by 14% of women who said they had an average risk for breast cancer.
In comparison, only 7% of women who said they had a low risk for developing breast cancer in the next decade underwent routine mammography. That percentage was a little higher than the 10% of women who thought they had no immediate risk of developing breast cancer at all.
6. Level of breast cancer fear
Finally, the researchers observed a statistically significant relationship between fear of breast cancer and mammography participation rates. One out of every four women (25%) with a high level of breast cancer fear said they underwent biannual mammography. The proportion of women who underwent routine mammography was much lower for those with moderate fear (6%) and little fear (4%).
Despite the relationship, the researchers found the level of fear actually had a negative influence on mammography usage in their logistic regression analysis. That analysis showed that women with a higher fear of breast cancer underwent mammography 5% less often than those with less fear.
"Psychosocial initiatives and planned counseling and education can help to reduce women's fear of cancer and perceived risk, and to increase their participation in screening behaviors," wrote Taylan, an associate professor of surgical nursing, and colleagues.
Key takeaways
It's important to note the study's screening population had some big differences from women in the U.S. For instance, only 9% of the women surveyed underwent biannual mammography, compared with 65% of U.S. women, according to data from the U.S. Centers for Disease Control and Prevention. In addition, 62% of women surveyed identified as housewives, and 27% had a high school or higher education.
The researchers plan to use the insights to improve their facility's health education, counseling, and case management, with the goal of increasing mammography usage and other behaviors that can help detect breast cancer early. They also called for future studies to further investigate some of the influential factors they found.
"Future studies can focus on the evaluation of shyness, the fear of mammography procedure, women's self‐efficacy, and giving priority to risk groups as perceived in interviews with women," they concluded.