3D models that combine vascular and biliary anatomy using different imaging techniques can contribute to more rigorous planning of complex liver operations, including hepatic resections, living-donor transplantation, vascular intervention procedures, and biliary reconstruction surgery, Portuguese researchers have reported at the RSNA 2020 meeting.
"Radiologists play a central role in this growing field and in close collaboration with referring clinicians, they can make 3D models a widely available reality in patient-focused medicine," noted Nuno Pereira da Silva and colleagues from the medical imaging department at Coimbra University Hospital.
 During the segmentation process, several techniques can be used to select the main structures, including thresholding, edge detection, region growing, and multiple-slice interpolation as well as manual segmentation with draw, paint, and erase/cut tools. 3D Slicer, an open-source software platform, was used for these models. All figures courtesy of RSNA 2020 and Nuno Pereira da Silva.
During the segmentation process, several techniques can be used to select the main structures, including thresholding, edge detection, region growing, and multiple-slice interpolation as well as manual segmentation with draw, paint, and erase/cut tools. 3D Slicer, an open-source software platform, was used for these models. All figures courtesy of RSNA 2020 and Nuno Pereira da Silva.Growing scientific evidence supports the benefits of 3D models in clinical practice. They can reduce surgical and anesthetic time and lead to a decrease in the number and severity of complications, shorter hospitalization time (and lower associated costs), and improvement in surgical precision due to better preoperative planning, resulting in better outcomes, the researchers explained in a digital poster.
The technology can also result in technical improvements through the possibility of simulation with appropriate models and in improved communication between healthcare professionals and patients.
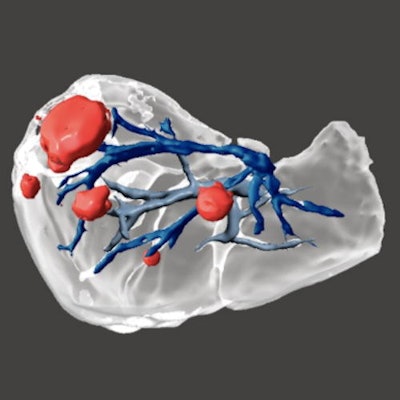
 Liver metastasis of colorectal carcinoma. Five liver metastases were identified on MRI with hepatospecific agent. The 3D model was useful for surgical planning due to the well established relationships between the metastasis and the vessels as well as the 3D positioning of the nodules within the liver.
Liver metastasis of colorectal carcinoma. Five liver metastases were identified on MRI with hepatospecific agent. The 3D model was useful for surgical planning due to the well established relationships between the metastasis and the vessels as well as the 3D positioning of the nodules within the liver.3D models are increasingly used to help surgeons, guiding them through the complex hepatic vasculobiliary anatomy. They can help in the resection of hepatic primary tumors and metastasis because they can demonstrate the location within hepatic segments and the relationship with adjacent structures such as hepatic and portal veins, arteries, and bile ducts.
3D models are useful in surgical planning, and optimal resection planes can be selected prior to surgery. In patients at risk of post-hepatectomy liver failure, liver volumes may be calculated for various possible resection approaches.
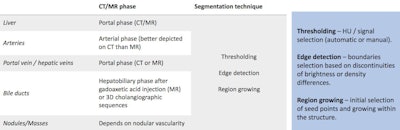 Segmentation techniques and postprocessing.
Segmentation techniques and postprocessing.The following five 3D printers are particularly suitable for liver applications:
- Jetted photopolymer: The photopolymer is deposited in drops on a platform to create layers that are solidified by ultraviolet (UV) light.
- Vat photopolymerization: A UV light is used to cure or harden the liquid photopolymer resin within a vat. As the platform moves, the object is made downward after each new layer is cured.
- Binder jetting: A liquid binding agent is selectively laid down to join powder particles in layers that are bound to form the object.
- Fused filament fabrication: An extrusion-based technique in which the filaments of a nozzle are deposited layer-by-layer to form the piece.
- Power bed fusion: This technique is used for hard plastic parts and is based on the selective fusing of materials in a granular bed. The parts are fused on a layer that moves upward in the working area, adding another layer of granules and repeating the process until the object has built up.
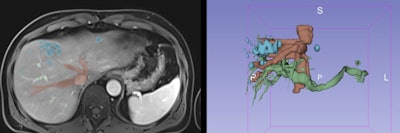
 Left images: 3D model for interventional planning in a 5-year-old boy with a congenital intrahepatic portosystemic shunt. Right images: 3D model after shunt closure with Amplatzer device (silver color) in a 4-year-old boy with a congenital portosystemic shunt.
Left images: 3D model for interventional planning in a 5-year-old boy with a congenital intrahepatic portosystemic shunt. Right images: 3D model after shunt closure with Amplatzer device (silver color) in a 4-year-old boy with a congenital portosystemic shunt.The development and availability of new virtual reality (VR) technologies in the near future may limit the need for printed models, the authors cautioned.
"Virtual surgical planning is a growing field, and virtual preoperative simulation may solve some ethical issues associated with medical education, as it is a learning tool for training procedures without potential harm to patients," they pointed out. "VR is also eco-sustainable and requires no use of plastics."



















