Medical imaging professionals must brush up on their ability to identify and diagnose hepatic pseudolesions on CT because of the close resemblance of pseudolesions to primary tumors and metastases of the liver, according to prizewinning research from Romania presented at ECR 2020 Online.
"In patients with cancer, some forms of pseudolesions can cause panic," noted Drs. Andrei Neagu and Cezar Betianu, from the department of radiology at Dr. Carol Davila Central Military University Emergency Hospital, Bucharest. "Therefore, an in-depth knowledge of liver hemodynamics and enhancement patterns is important in judging whether an abnormal finding is induced by a true lesion."
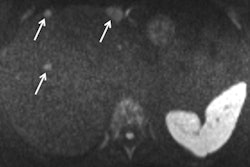
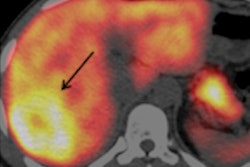
 Caudate lobe hypertrophy in a patient with portal cavernoma. If suspected, a follow-up CT may be done to change the association between the rib/diaphragm and adjacent liver at a different inspiration level or with the patient in a decubitus position. All images courtesy of Drs. A.V. Neagu and C.-I. Betianu, originally presented at ECR 2020.
Caudate lobe hypertrophy in a patient with portal cavernoma. If suspected, a follow-up CT may be done to change the association between the rib/diaphragm and adjacent liver at a different inspiration level or with the patient in a decubitus position. All images courtesy of Drs. A.V. Neagu and C.-I. Betianu, originally presented at ECR 2020.Pseudolesions tend to have a typical appearance, but there are many cases with atypical patterns, explained Neagu and Betianu, who received a cum laude award from the ECR 2020 e-poster judges.
The team urged all radiologists to learn more about the etiology, pathophysiology, and ultrasound, CT, and MRI appearance of hepatic pseudolesions, as well as finding out about how to recognize vascular anatomical variants on various imaging studies and how to discriminate pseudolesions from true lesions. CT and ultrasound have a useful diagnostic role, but MRI appears to be the more sensitive in solving more complex problems.
Pseudolesions of the liver are nonneoplastic abnormalities and can cause parenchymal and vascular changes. They often occur due to blood flow abnormalities, and they can be found in both cirrhotic and noncirrhotic livers. The liver has dual blood supply, with the portal vein carrying 75% of blood and the hepatic artery with 25% of blood and a drainage route through the hepatic veins.
The authors pointed out that pseudolesions can be divided into focal mass-like parenchymal change normal liver function and focal mass-like findings on imaging without parenchymal change.
"Thorough knowledge is useful in discriminating if an abnormal imaging finding is induced by a true lesion," they stated.
Fat accumulation is one of the most common conditions of the liver, and fatty liver is characterized by the accumulation of triglyceride droplets in hepatocytes not in the extracellular matrix. Focal fatty change (FFC) is related to veins of the third inflow, which carry blood richer in various hormones that dilute regional portal flow and induce ischemia. Both factors contribute to fat accumulation.
"Conversely, focal sparing regions are perfused by veins of the third inflow poorer in dietary elements absorbed in the small intestine. This may cause areas of focal sparing in a diffuse fatty liver," Neagu and Betianu wrote. "There are common areas for both FFC and focal sparing and uncommon areas like perivascular and perilesional."
Awareness of inflammatory pseudotumors (IPTs) is important too. These rare benign lesions are of unknown origin, but the primary cause is thought to be occlusive phlebitis or an undetected incautious agent. They occur most commonly in the lung and orbit, but they have been reported at nearly all body sites.
Most cases are solitary, well-circumscribed, encapsulated solid tumors, mainly arising from the right hepatic lobe. The lesions are more common in men than women, especially young adults. Clinical manifestations are acute inflammatory process and recurrent pyogenic cholangitis
"The differential diagnosis of liver masses is crucial because IPTs can mimic malignant tumors. The radiologist should be familiar with this entity and help avoid unnecessary surgery when possible," Neagu and Betianu noted.
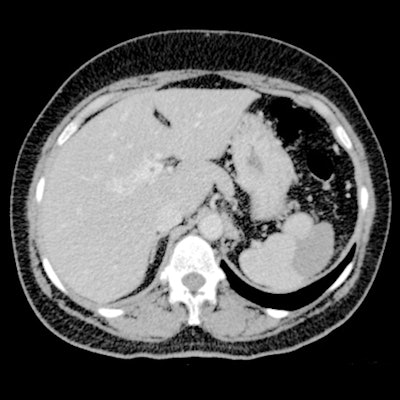
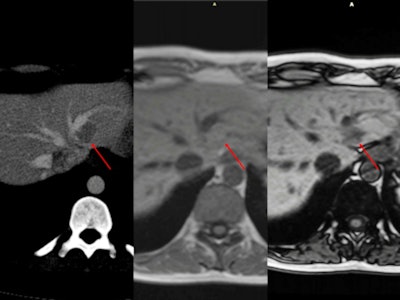 Multifocal fatty liver with no obvious relationship to vascular flow. CT scan shows multiple regions of hypoattenuation on unenhanced CT and portal phase (arrow). When the same patient underwent an MRI scan for follow-up, there was no restricted diffusion. Gradient-echo imaging demonstrates intracellular fat with a drop of signal on out-of-phase images.
Multifocal fatty liver with no obvious relationship to vascular flow. CT scan shows multiple regions of hypoattenuation on unenhanced CT and portal phase (arrow). When the same patient underwent an MRI scan for follow-up, there was no restricted diffusion. Gradient-echo imaging demonstrates intracellular fat with a drop of signal on out-of-phase images.Peliosis hepatis is a rare entity characterized by blood-filled cystic cavities (< 1 mm to several cm in diameter) distributed randomly throughout the liver. First described in patients with advanced cancer and tuberculosis and users of anabolic steroids, its imaging findings vary with the size of lesions, presence or absence of thrombus within the cavities, and presence of hemorrhage, they added. The microscopic form has no specific characteristics.
Confluent hepatic fibrosis is generally caused by chronic injury to the liver patients with long-standing cirrhosis and vascular injury to the liver.
Knowledge of the radiologic appearance of arterioportal fistulas is also important, according to the authors. Portosystemic shunts comprise abnormal cystic or tubular anechoic structures communicating between portal venous branches and hepatic veins. Both extrahepatic and intrahepatic portosystemic shunts have been described.
Editor's note: To view the authors' full e-poster and clinical images, go to the European Society of Radiology's EPOS website.