FDG-PET/CT can be an effective tool when it comes to breast cancer staging and treatment evaluation, but it still shouldn't be used for diagnosis, a Spanish expert told attendees at a webinar held on 28 May by the European Society for Hybrid, Molecular, and Translational Imaging (ESHIMT).
Clarifying the applications of the modality is central to making the best use of it, said presenter Dr. José Vercher-Conejero of Bellvitge University Hospital in Barcelona, Spain.
 Dr. José Vercher-Conejero.
Dr. José Vercher-Conejero."In daily clinical practice, we sometimes find ourselves faced with dilemmas such as what imaging tests we could do for this or that application. Professional guidelines help a lot -- they are basic and essential -- but each center can have its own [practice factors] and I think that we must know how to adapt ourselves and make best use of the technique we have for each situation," he told AuntMinnieEurope.com via email.
In his presentation, Vercher-Conejero offered delegates a "state of the modality" update on using FDG-PET/CT for breast cancer, covering everything from diagnosis to disease recurrence.
State of the modality
FDG-PET/CT can be an effective tool in the imaging arsenal, but there's a catch, Vercher-Conejero cautioned: Radiologists must be aware of normal biodistribution of FDG in the body, since its uptake is not specific to cancer cells.
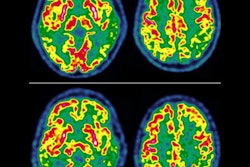
"Any cell ... with transporters that metabolize glucose may take up FDG and appear avid," he said. "These include normal cells such as myocardial cells, hepatocytes, and neurons and nonneoplastic processes, most notably infection and inflammation."
It's also important to understand what causes false positives on FDG-PET/CT, such as dysplasia, fibroadenomas, ductal ectasia, inflammation, silicone leaks from breast augmentation, and fat necrosis; false negatives can be caused by lesions less than 1 cm, tubular or lobular carcinoma, or carcinoma in situ, Vercher-Conejero said. Dense breast tissue, the menstrual cycle, and lactation can confuse PET results as well, he noted.
Best practices
These caveats suggest that FDG-PET/CT's use for breast cancer must be clearly defined. Vercher-Conejero outlined current recommendations for the use of the modality, citing guidance from three professional organizations: the European Society for Medical Oncology (ESMO), the National Comprehensive Cancer Network (NCCN), and the National Institute for Health and Care Excellence (NICE).
Initial lymph node diagnosis. Full-body FDG-PET/CT has limited value for this purpose, due to its lower sensitivity than some other modalities. It is not recommended for breast cancer diagnosis, as its capabilities are limited by the size of lesions (around 1 cm) and the fact that it is less sensitive to invasive lobular carcinoma and slow-growing cancers, and it should not be substituted for axillary nodal dissection and sentinel node biopsy, he said.
Staging. FDG-PET/CT can be helpful for local staging when standard imaging results are unclear, according to Vercher-Conejero. In regards to staging distant disease, Vercher-Conejero cited one study that found that the modality caused clinicians to adjust patients' disease stage a third of the time (Journal of the National Cancer Institute, December 19, 2012, Volume 104:24, pp. 1879-1887).
Treatment response. FDG-PET/CT may be helpful in monitoring the chemotherapy or hormonal therapy responses of patients. "Poor response on PET translates to treatment failure," he said.
Disease tracking and relapse/recurrence. FDG-PET/CT can be used to make new diagnoses of metastases in patients with breast cancer with imaging suspicious of metastatic disease but not necessarily diagnostic, Vercher-Conejero said, but it should not be used to monitor advanced breast cancer. As for relapse or recurrence, the recommendation again is to use FDG-PET/CT when other imaging is equivocal.
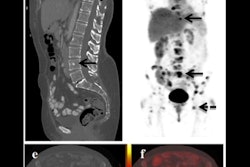
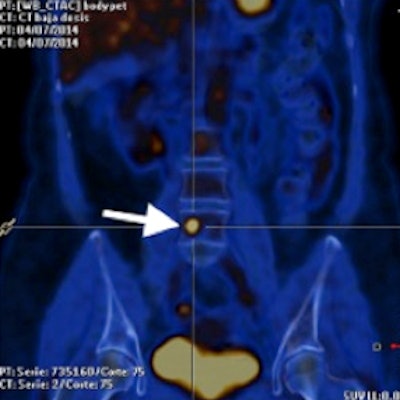
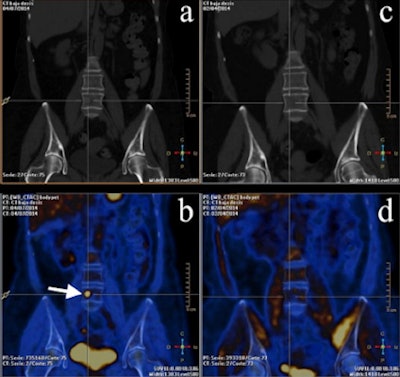 PET/CT images from a 53-year-old woman with breast cancer in the course of therapy but with rising biomarkers. (a, b) PET/CT images midtherapy. (c, d) Basal PET/CT images. Bone M1 can only be seen with FDG-PET. Images courtesy of Dr. José Vercher-Conejero.
PET/CT images from a 53-year-old woman with breast cancer in the course of therapy but with rising biomarkers. (a, b) PET/CT images midtherapy. (c, d) Basal PET/CT images. Bone M1 can only be seen with FDG-PET. Images courtesy of Dr. José Vercher-Conejero.Future directions
Finally, Vercher-Conejero listed a number of FDG-PET trends to watch for in the breast cancer imaging arena.
- The increased use of artificial intelligence (AI) with FDG-PET/CT
- "New" radiotracers for additional breast cancer evaluation: F-18 sodium fluoride (NaF) for bone imaging; F-18 fluoroethylcholine (FECH) and F-18 fluoromisonidazole (FMISO) for hypoxia; F-18 fluoroestradiol (FES) for hormone receptors, specifically estrogens; and F-18 fluorothymidine (FLT) for cell proliferation
- Positron emission mammography (PEM) as a complement to mammography; fused PEM and mammography images
- Digital PET, which uses silicon-based photodiodes instead of traditional photomultiplier tubes
- Combined PET/MR technology
It's well worth the effort to stay up-to-date on the use of FDG-PET/CT for breast cancer, according to Vercher-Conejero.
"It's important to review the latest recommendations offered by the clinical guidelines, [continue to discuss] advances in medical imaging, and to refresh already known concepts about how PET/CT can help in the management of breast cancer patients," he told AuntMinnieEurope.com.