The combination of 3D printing and virtual reality (VR) technology can enable anesthesiologists to produce a personalized and more appropriate airway plan for lung operations on pediatric patients, researchers stated in a new case report published in the European Journal of Anaesthesiology.
A team from Tel Aviv Sourasky Medical Center in Tel Aviv, Israel, used CT images to produce a 3D-printed model of a 7.5-year-old patient's airway anatomy. After performing a virtual bronchoscopy and then practicing on a 3D-printed model, an anesthesiologist created a new airway plan that was much better suited to the specific anatomy of this pediatric patient than a plan based on just CT measurements.
"The final airway plan was substantially different to the plan developed using standard imaging techniques," wrote the authors, led by Dr. Ruth Shaylor. "This reduced the number of attempts at lung isolation that would have been performed on the patient."
A challenging case
The young girl had been scheduled for right upper lobectomy for a lung metastasis from a Ewing's Sarcoma. However, her anesthesiologists were concerned that conventional tubing and devices used for lung operations in older patients may not be appropriate for pediatric cases (European Journal of Anaesthesiology, June 2020, Vol. 37:6: pp. 508-515).
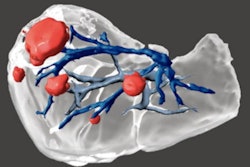
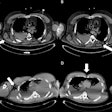
To reduce the potential for trial and error in airway manipulation during the surgery, the researchers developed a 3D model by identifying the trachea, bronchi, and lobar bronchi on a patient's existing CT scan using IntelliSpace Portal v11 (Philips Healthcare). These images were then imported into 3-matic Medical 14.0 postprocessing software (Materialise).
After the walls of the model were built outward to maintain the internal diameter and hollowed out to test one-lung ventilation, the model was then printed in clear hard plastic on a PolyJet J750 printer (Stratasys). It was also converted into the Dicom to Print (D2P) VR program from 3D Systems in order to facilitate a virtual bronchoscopy.
 3D-printed model of 7.5-year old patient's airway. All images courtesy of Dr. Ruth Shaylor.
3D-printed model of 7.5-year old patient's airway. All images courtesy of Dr. Ruth Shaylor.Prior to using the 3D model, the treating anesthesiologist used standard CT measurements to develop an initial airway plan, which consisted of a 26-French gauge double-lumen tube as Plan A and a 5‑mm microlaryngeal tube as Plan B.
A new, better plan
After getting to know the patient's airway on a VR simulator and then testing different equipment on the 3D-printed model, the anesthesiologist changed the final airway plan to a 5-mm endotracheal tube and bronchial blocker as the Plan A and a 5-mm microlaryngeal tube directed into the left main bronchus as the Plan B.
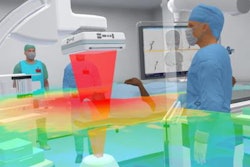
 A virtual bronchoscopy enabled better understanding of the patient's airway anatomy.
A virtual bronchoscopy enabled better understanding of the patient's airway anatomy.After induction of anesthesia in the patient, the trachea was intubated with a 5-mm endotracheal tube and lung isolation was achieved on the first attempt using a bronchial blocker with fiber-optic guidance, according to the researchers. The anesthesiologist found that the patient's anatomy correlated well with the virtual reality model, enabling the carina and right upper lobe bronchus to be easily identified.
"In the current case, the treating anesthesiologist reported the virtual reality bronchoscopy to be useful in identifying airway structures and ensuring correct placement of the [endotracheal tube]," the authors wrote. "In addition, it helped to confirm the position of the [right upper lobe bronchus] when placing the bronchial blocker."
Complete airway blockade and collapse of the lung were achieved throughout the surgery. The patient was extubated at the end of the procedure and went on to make an uneventful recovery, according to the authors.
Underutilized in anesthesia
The researchers said that both 3D printing and VR are underutilized for patient-specific preoperative planning in anesthesia.
"We successfully combined both technologies to produce a [personalized] airway plan for a [pediatric] patient," they wrote.
The researchers noted that their method might be considered by experienced pediatric thoracic surgery teams to be "overkill." However, thoracic anesthesiologists less familiar with one-lung ventilation in pediatric patients can quickly and safely add experience by preparing this type of a personalized airway model, they said.