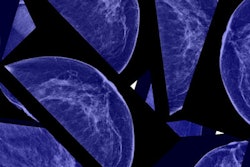
In a large cohort, German researchers observed a reduction in late-stage breast cancer incidence and mortality in women screened for breast cancer, which can most likely be attributed to the national mammography screening program, they said. In addition, they noticed only a moderate occurrence of overdiagnosis.
The group, led by Dr. Alexander Katalinic from the Institute for Social Medicine and Epidemiology at the University of Lübeck, sifted through data on more than 323,000 breast cancer patients over a 10-year period, covering a population of 30 million.
In brief, they concluded that breast cancer screening is effective.
"We conclude that the observed trend changes in breast cancer mortality, with continuing decline in the screening-exposed group and not in the nonexposed groups, fit very well with expected effects of an effective mammography screening," the authors wrote (International Journal of Cancer, 1 November 2019).
Screened vs. not screened
To determine whether a mammography screening program is effective, several outcomes must be observed, they explained:
- Breast cancer incidence should show an initial short-term increase (prevalence peak) with a following decline.
- After several years, the incidence of late-stage breast cancer should decline below the prescreening level.
- Breast cancer mortality should decrease in the long term.
The researchers used these criteria to determine the effectiveness of Germany's national breast screening program, which was introduced in 2005. Specifically, they analyzed total and stage-specific breast cancer incidence and mortality in screened and unscreened women before and after the German program was implemented.
Katalinic and colleagues used data from 2003-2004 for their prescreening period. After that, women ages 50 and older were invited to screen every two years. They used official mortality data from 1998 to 2016 for almost the whole of Germany, along with information on 323,719 breast cancer patients across regions from 2003 to 2014. To compare incidence rates, the researchers used the latest available data from 2013-2014, while for mortality rates, the data were from 2015-2016.
From 2003-2004 to 2015-2016, breast cancer mortality decreased by 25.8% in the 50- to 59-year age group and by 21.2% in the 60- to 69-year age group.
| Breast cancer mortality rate in Germany per 100,000 women | |||
| Age group | Before screening | After screening | Percent change |
| 50-59 | 48.9 | 36.3 | 25.8% |
| 60-69 | 79.9 | 62.9 | 21.2% |
Breast cancer incidence showed a typical prevalence peak with the introduction of breast screening, mainly driven by an increase in the detection of early-stage breast cancer, while cases of late-stage cancer fell.
| Breast cancer incidence rate in Germany per 100,000 women | |||
| Age group | Cancer stage | Before screening | After screening |
| 50-59 | DCIS* | 15.7 | 40.3 |
| I | 90.7 | 119.1 | |
| II | 89.0 | 90.2 | |
| III | 35.5 | 27.0 | |
| IV | 16.6 | 12.8 | |
| 60-69 | DCIS | 17.4 | 46.1 |
| I | 118.5 | 171.9 | |
| II | 111.9 | 109.7 | |
| III | 47.5 | 34.1 | |
| IV | 25.5 | 19.3 | |
Katalinic and colleagues observed no change or substantially smaller changes in the age groups that did not receive screening.
"The reduction of late-stage breast cancer incidence and breast cancer mortality in the screening-exposed age groups in Germany is most likely to be attributed to the introduction of the national mammography screening program," they noted.
Furthermore, age-standardized breast cancer mortality was 26.7/100,000 in the years before the mammography program was introduced and 23.2/100,000 after it was established.
Overdiagnosis and limitations
The incidence of invasive breast cancer almost fell to the level of the prescreening period during the 10-year time span of the study, but ductal carcinoma in situ (DCIS) remained substantially elevated. An excess of total incidence (in situ and invasive carcinomas) after introducing screening might indicate overdiagnosis, according to the authors.
"Based on a period of 10 years after the start of the breast cancer screening program and assuming no underlying secular incidence trends, our results suggest a screening-related excess in total breast cancer incidence of 17%-19% in the screening age groups, reflecting a moderate fraction of overdiagnosed breast cancers," they wrote. "This result is in the range reported from randomized controlled trials or cohort studies (10%-22% and 1%-36.2% respectively)."
Linked with overdiagnosis is often the question of whether a change in risk factors, such as hormone replacement therapy and obesity, would have naturally sunk breast cancer rates.
"Hypothesizing such changes, however, they should have similar effects on all stages and are therefore incapable to explain isolated effects on late-stage breast cancer. ... In our case, the decline of advanced breast cancer was isolated to the screening-exposed age group making other factors improbable," the authors explained.
Katalinic and colleagues concluded that even if the evidence level of their observation is limited, a causal relationship between the implementation of the mammography screening program in Germany and the observed stage-specific trends seems likely.
"All in all, declining advanced stage and increasing early-stage breast cancer incidence in the screening age groups, but not in the others ... paint a consistent picture of the expected effects on stage-specific incidence after the introduction of an effective screening program," they wrote.