The epidemic of nonalcoholic steatohepatitis (NASH) in children is evolving even faster than that of obesity, according to a presentation at the French national radiology congress (JFR) in Paris. In the adult population, NASH has become one of the leading indications for liver transplantation in some countries; therefore, tools to detect and grade NASH in children are crucial for providing good follow-up and avoiding poor outcomes.
Better detection of NASH in the pediatric population should become possible in the coming years, thanks to the development of tools such as multiparametric quantitative ultrasound and MRI, according to Dr. Stéphanie Franchi-Abella, PhD, head of pediatric interventional radiology at Bicêtre Hospital in Le Kremlin-Bicêtre.
In a presentation on Saturday morning during the session on NASH in children and adults, Franchi-Abella outlined how behavioral changes leading to obesity in children and teenagers mean that nonalcoholic fatty liver disease (NAFLD) has become an important cause of chronic liver disease in children, with a prevalence ranging from 3% to 10% in the general population and up to 70% in obese children.
"The challenge is to be able to detect liver steatosis and to distinguish patients with simple steatosis from those who evolve to NASH that associates steatosis with inflammation and a ballooning of the hepatocytes and may evolve to cirrhosis and/or hepatocellular carcinoma," she said. "Moreover, NASH is associated with diabetes mellitus [type] 2 and metabolic syndromes, which require specific management."
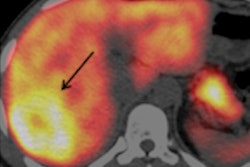
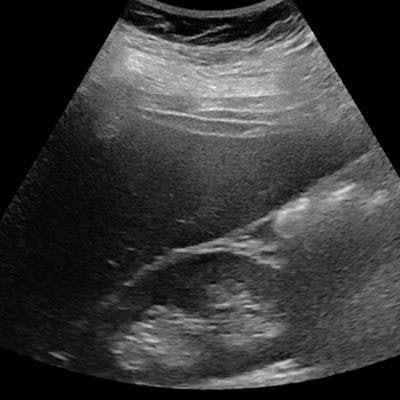
![Ultrasound of a 14-year-old girl with severe obesity (body mass index [BMI], 42 kg/m2). There is hepatomegaly associated with increased liver echogenicity when compared to the right kidney and attenuation corresponding to severe steatosis. Below, the same patient shows increased liver-to-kidney ratio. All images courtesy of Dr. Stéphanie Franchi-Abella, PhD.](https://img.auntminnieeurope.com/files/base/smg/all/image/2019/10/ame.2019_10_10_21_09_1189_steatose-fig-1a.png?auto=format%2Ccompress&fit=max&q=70&w=400) Ultrasound of a 14-year-old girl with severe obesity (body mass index [BMI], 42 kg/m2). There is hepatomegaly associated with increased liver echogenicity when compared to the right kidney and attenuation corresponding to severe steatosis. Below, the same patient shows increased liver-to-kidney ratio. All images courtesy of Dr. Stéphanie Franchi-Abella, PhD.
Ultrasound of a 14-year-old girl with severe obesity (body mass index [BMI], 42 kg/m2). There is hepatomegaly associated with increased liver echogenicity when compared to the right kidney and attenuation corresponding to severe steatosis. Below, the same patient shows increased liver-to-kidney ratio. All images courtesy of Dr. Stéphanie Franchi-Abella, PhD.Early detection is important, as diet may reverse the process at the early phase of the disease. Yet the detection and quantification of liver fat content and associated fibrosis and inflammation, mandatory in the diagnosis of NASH, remain challenging in children; B-mode ultrasound remains relatively limited for the diagnosis of liver steatosis, as fat content should be more than 20%, but quantification is not yet available as a routine clinical tool on ultrasound scanners, according to Franchi-Abella.
Although liver fibrosis evaluation is improving with the use of shear-wave elastography (SWE), it still lacks validation for pediatric use. Meanwhile, MR quantification of steatosis and fibrosis remains difficult in children and less effective than in adults.
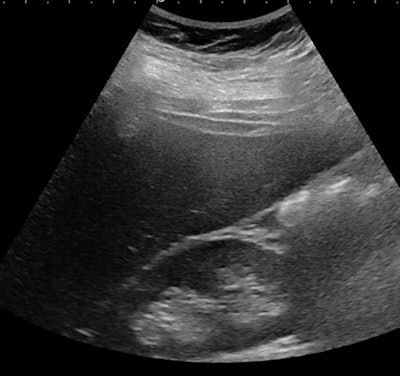 Ultrasound of a 16-year-old girl with severe obesity (BMI, 51 kg/m2) but no increase in liver echogenicity. She was considered not to have liver steatosis.
Ultrasound of a 16-year-old girl with severe obesity (BMI, 51 kg/m2) but no increase in liver echogenicity. She was considered not to have liver steatosis.Light on the horizon
There is light on the horizon, however. Recent developments in ultrasound technology may improve the quantification of fat content using the controlled attenuation parameter (CAP), while SWE techniques can help assess fibrosis and inflammation, the latter through viscosity evaluation.
 Dr. Stéphanie Franchi-Abella, PhD, from Bicêtre Hospital.
Dr. Stéphanie Franchi-Abella, PhD, from Bicêtre Hospital."At present, the gold standard for the diagnosis of NASH in pediatric patients remains liver biopsy, which is both imperfect and invasive. That is why a huge effort is being made to develop noninvasive evaluation of these disorders," Franchi-Abella said. "By building scores using lab tests and performing B-mode [ultrasound] and ultrasound quantification with CAP and SWE, we may greatly improve the detection of early NAFLD and low grades of fibrosis in NASH patients."
Of course, the improvement of MRI techniques will also be very important, she added. In the adult population, MRI provides the most precise quantification of hepatic fat content, especially when using proton density fat fraction (PDFF) quantification sequences in clinical routine -- and spectroscopy in research centers. Hepatic MR elastography also has good results for detecting fibrosis in these patients.
However, results, including those from MR elastography, are less than optimal in the pediatric population, mainly for two reasons: first, because of technical issues for the youngest patients who need sedation and for whom automatic segmentation for the quantification of fat content may be difficult. Second, NASH in children and teenagers is different from the disease in the adult population, with less inflammation that is predominantly periportal and less fibrotic.
"We will have to select the population that requires specific detection: overweight and obese patients and, due to hereditary factors, also siblings of patients with NASH, because around 59% of siblings are also affected," she said.