Bowel ultrasound scans may be able to predict which children need second-line treatment for acute severe colitis, according to a study published on 25 February in the Journal of Pediatric Gastroenterology and Nutrition.
Acute severe colitis is a life-threatening emergency that requires rapid, aggressive medical treatment -- first with intravenous steroids, then with infliximab or calcineurin inhibitors if needed.
The new study suggests that features on ultrasound scans may be able to help predict which patients require second-line therapy. The hope is that prompt second-line treatment could result in early discharge or even prevent a colectomy.
"This is the first study investigating the potential prognostic role of [bowel ultrasound scan] in pediatric [acute severe colitis]," wrote the team of Italian authors, led by Dr. Luca Scarallo from the University of Florence. "These results highlight the potential role of [bowel ultrasound scan] in adding relevant prognostic information to clinical evaluation in pediatric [acute severe colitis]."
Children are at a greater risk for hospitalization due to acute severe colitis than adults. For patients with this condition, doctors first prescribe a five-day course of intravenous methylprednisolone. However, this first-line treatment doesn't work for many patients.
The authors wondered whether features on bowel ultrasound scans could be used to distinguish children who might need second-line treatment with infliximab or calcineurin inhibitors before their five-day, first-line treatment ends.
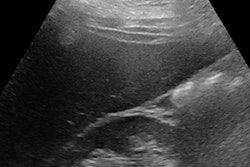
To find out, they looked at 69 cases of children with acute severe colitis who were admitted to a children's hospital in Florence, Italy, between 2008 and 2018. The children were given steroids as their initial treatment. They also underwent a bowel ultrasound scan performed by two experienced pediatric radiologists on the third day of their hospital stay.
About half of the children in the study did not respond to steroid therapy and required a second-line treatment. A further 12 children didn't respond to either treatment and required urgent colectomy.
A total of 47% of children who required second-line acute colitis treatment showed loss of colonic wall stratification (CWS) on ultrasound scans. In contrast, only one of the children who responded to the first-line treatment had CWS loss.
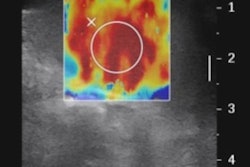
In addition, the majority of cases (86%) that required second-line treatment showed enhanced vascularization, compared with under half of the cases (45%) for those who responded to steroids. Children who needed second-line treatment also showed significantly worse colonic wall thickness measurements on ultrasound scans, with an average thickness of 1.45 mm greater than those who responded to the first-line treatment.
The predictive value of the need for second-line treatment was even higher when the authors combined the ultrasound scan findings with a Pediatric Ulcerative Colitis Activity Index (PUCAI) score of greater than 45 on the third day of hospitalization. The combined analysis demonstrated a specificity of 97% and a positive predictive value of 94%.
"Loss of CWS assessed at [bowel ultrasound scan] may be helpful to integrate information provided by PUCAI score and to allow establishing a lower threshold for the initiation of second-line treatment," Scarallo and colleagues wrote. "This approach may contribute to spare steroid therapy and possibly allow earlier discharges."
The authors noted that they didn't find any significant associations between ultrasound scan findings and children who needed a colectomy. Furthermore, ultrasound scans can be a time-consuming and expensive modality that requires an experienced operator. As a result, the findings need to be confirmed through larger, multicenter studies.
"Our study, despite its limitations, indicated that [bowel ultrasound scan] may represent an effective noninvasive tool to predict first-line therapy failure in patients with [acute severe colitis], providing potentially critical information for the clinician to tailor the management of these patients, allowing a better-targeted therapy," they concluded.