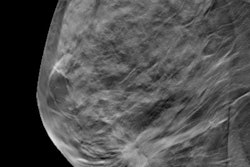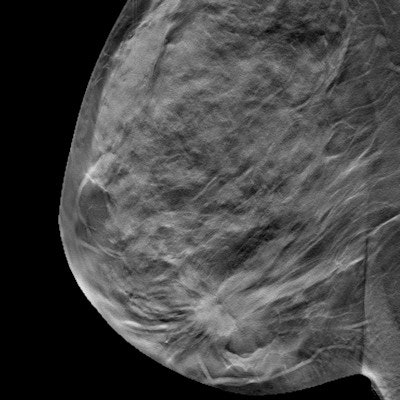
Lower recall and higher cancer detection rates for breast cancer screening with digital breast tomosynthesis (DBT) are sustainable over more than one screening round, according to an extensive Norwegian study published online on 11 June in European Radiology.
The research addresses a knowledge gap about DBT's ongoing performance compared to digital mammography (DM), wrote a team led by Dr. Tone Hovda of Vestre Viken Hospital in Drammen.
"There is limited knowledge about early performance measures for screening with digital breast tomosynthesis beyond one screening round," the group wrote.
Previous research has suggested that DBT is a more sensitive screening tool for breast cancer than DM. Yet in these studies, DBT was used in combination with DM and evaluated for only one screening round. Hovda and colleagues sought to assess the modality's performance as a standalone screening tool over more than one screening round.
To do so, they evaluated data from 35,736 women screened in Norway's BreastScreen program between 2008 and 2016 who underwent at least two consecutive screening rounds. The screening technique changed during the study period, so the cohort was divided into four groups:
- DM after DM
- DBT after DM
- DM after DBT
- DBT after DBT
DBT performed well compared with DM over multiple screening rounds across a variety of measures, the researchers found.
| DM, DBT performance over multiple screening rounds* | ||||
| Performance measure | DM after DM | DBT after DM | DM after DBT | DBT after DBT |
| Cancer detection rate per 1,000 women screened | 4.6 | 9.9 | 4.3 | 8.3 |
| PPV1 (positive screening result) | 12.9% | 36.4% | 20% | 43.5% |
| Recall rate | 3.6% | 2.7% | 2.2% | 1.9% |
| Sensitivity | 67.6% | 83.7% | 62.9% | 80.2% |
| Specificity | 96.9% | 98% | 98.6% | 98.9% |
In addition, there were no statistically significant differences in the interval cancer rates between the study groups, and tumor characteristics tended to be prognostically favorable for DBT compared with digital mammography.
"We found a lower recall among women screened with DBT after DM compared with DM after DM, but even lower among those with a prior DBT," the team noted. "The highest rates of screen-detected breast cancer were observed among women screened with DBT after DM or consecutive DBTs."
Overall, the investigation suggests that DBT performs well over multiple screening rounds -- although further research across even more rounds is needed, according to Hovda and colleagues.
"Our study showed that recall remained lower and screen-detected breast cancer higher for consecutive screening examinations with DBT versus standard DM," they wrote. "Whether our results remain stable over several more screening rounds is yet to be investigated."
Both a long-term increased rate of screen-detected breast cancer and a reduction in the rate of interval cancer are crucial when considering DBT as a sustainable and more effective tool for mammographic screening than standard DM alone, they concluded.