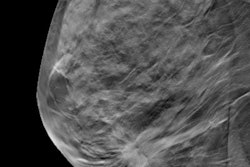
Researchers from Norway have found that breast cancer screening with digital breast tomosynthesis (DBT) plus synthesized 2D mammography performs comparably to digital mammography and can safely be used alone in population-based screening programs. Their study of nearly 29,000 women was published on 8 May in Lancet Oncology.
 Solveig Hofvind, PhD.
Solveig Hofvind, PhD.This research adds further support for the use of DBT as a breast cancer screening modality, noted the team led by Solveig Hofvind, PhD, head of the Norwegian Breast Cancer Screening Program since 2013 and radiography professor at Oslo Metropolitan University (formerly Oslo and Akershus University College of Applied Sciences).
"Our population-based, breast cancer screening trial using first-generation digital breast tomosynthesis with synthetic 2D mammogram versus digital mammography alone did not identify a significant difference in the proportion of screen-detected breast cancer. ... Our results indicate that use of digital breast tomosynthesis in a screening setting is safe for women at average risk of breast cancer," the group wrote.
Varied effects
Previous research has shown that the combination of digital mammography and DBT increases cancer detection, but some European studies have demonstrated varied effects on the recall rate, Hofvind's group noted. The researchers sought to explore how DBT using synthesized 2D mammograms in Norway's screening program would perform on its own, compared with digital mammography.
The study included 28,749 women who attended the BreastScreen Norway program in Bergen between January 2016 and December 2017. Women were randomized into two study arms, one using DBT with synthesized 2D mammography images and the other using digital mammography. Eight radiologists interpreted the exams.
Of the total cohort, 14,380 women underwent DBT and 14,369 underwent digital mammography. The primary outcome assessed was the number of screen-detected breast cancers by screening technique. Secondary outcomes included percentage of recalls, positive predictive value of recall (PPV1) and biopsy (PPV2), and tumor characteristics.
Hofvind and colleagues found no statistically significant difference in the proportion of screen-detected breast cancer between the two modalities, except for the recall rate, which was significantly lower with DBT, and the positive predictive value of recall, which was higher with DBT. There also was no significant difference in tumor characteristics.
| DBT vs. digital mammography for breast cancer screening | |||
| Measure | Digital mammography (n = 14,369) | DBT (n = 14,380) | p-value |
| Screen-detected breast cancers | 87 | 95 | 0.56 |
| Ductal carcinomas in situ | 16 | 15 | 0.86 |
| Invasive cancers | 71 | 80 | 0.47 |
| Recall rate | 4% | 3.1% | < 0.0001 |
| PPV1 | 15.2% | 21.4% | 0.01 |
| PPV2 | 32.1% | 37.7% | 0.18 |
| Biopsy rate | 1.9% | 6.3% | 0.40 |
DBT also reduced the need for consensus consultations: The eight readers held consensus meetings for 6.3% of the DBT exams, compared with 7.4% of the digital mammography exams. However, interpretation time was longer for DBT, averaging one minute and six seconds instead of 39 seconds for digital mammography exams. This difference was perhaps due to insufficient experience in screen reading DBT exams and was a limitation of the study, the team wrote.
Further proof?
Yet, overall, the research suggests that DBT is a safe breast cancer screening tool, although more investigation is necessary, particularly regarding the incidence of interval cancers, according to Hofvind and colleagues.
"We found that use of digital breast tomosynthesis in a screening setting is safe, and has the potential to reduce harms, but studies on interval and screen-detected breast cancer in consecutive screening rounds are needed to better understand the effect of digital breast tomosynthesis in a population-based screening setting," they wrote.
The study also highlights the issue of how to incorporate new technology into clinical practice, wrote Dr. Sophia Zackrisson, PhD, of Lund University in Malmö, Sweden, in an accompanying editorial.
"Given that this is the first randomized trial of this technology, it has the potential to contribute important future information on interval cancers," she wrote. "[But it also] illustrates the complex interplay between new techniques and human readers in high-volume screening, and the challenges we will face in a possible future implementation phase of a new technology."