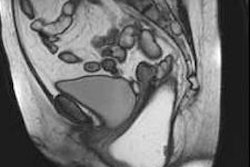
Award-winning research from Italy has underlined the clinical relevance of T2-weighted MRI as an important diagnostic tool to identify patients with parametrial invasion (PMI) in the preoperative assessment of cervical cancer.
The evaluation of PMI based on T2-weighted imaging helps in accurately stratifying patients with cervical cancer, both to determine the most appropriate management -- surgery, chemotherapy, or adjuvant treatment after surgery -- and to ensure the best clinical post-treatment outcomes, according to Dr. Barbara Sghedoni, Dr. Federica Fiocchi, and colleagues from the department of radiology at the University of Modena Policlinic. They won a prestigious magna cum laude award for their e-poster presentation at ECR 2019 in Vienna.
"The prognostic importance of PMI is well-known because it is associated with lymph node metastasis and disease-free survival," they noted. "Patients without PMI can be treated with less-aggressive treatments, while those with PMI undergo chemo-radiotherapy or require adjuvant therapy after surgery."
Furthermore, the evaluation of PMI is difficult by means of a clinical examination, depending on the extent of tumor invasion, and studies have reported an accuracy of between 29% and 53%, while MRI can depict PMI with an accuracy of up to 97%, they added.
Common malignancy
Uterine cervical cancer is the most common gynecologic malignancy and the second most common cancer in women worldwide in terms of incidence and mortality, the researchers wrote. The use of imaging is now complimentary to the clinical examination to assess important prognostic factors such as tumor size, parametrial extension and pelvic sidewall invasion, adjacent organ invasion, and the evaluation of lymph node metastases.
CT has limited use in local staging but can delineate enlarged lymph nodes, hydronephrosis, and distant metastases, and it permits complete whole-body staging in a single exam and simultaneous intravenous contrast media administration, they continued. MRI, on the other hand, can define both the local extent of the primary tumor and metastatic spread in the pelvis, delineating tumor size, parametrial and pelvic sidewall invasion, bladder or rectal infiltration, and lymph nodes metastases, due to its optimal soft-tissue contrast resolution.
The intactness of the cervical stromal rim on T2-weighted imaging, known as the hypointense rim sign, has shown excellent negative predictive value of 94% to 100%, enabling the identification of patients who are suitable for radical surgery, which is contraindicated in patients with PMI, added Sghedoni and colleagues.
"With disruption of the stromal ring without definite parametrial mass, there may be microscopic invasion understaged by MRI (false-negative findings)," they stated. "Linear stranding around the cervical mass is suggestive of PMI but may be due as well to peritumoral inflammatory tissue and can be a limitation of MRI, leading to an overstaging of the cervical pathology (false-positive findings)."
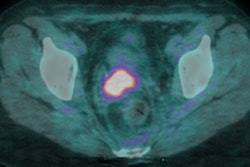
In addition to T2-weighted imaging, the apparent diffusion coefficient (ADC) mapping derived from diffusion-weighted imaging (DWI) on MRI is a promising emerging technique in the evaluation of cervical cancer, the authors pointed out.
Study goals
To evaluate the diagnostic value of T2-weighted imaging and ADC in predicting the presence or absence of PMI, 14 patients with newly diagnosed uterine cervical cancer that was pathologically confirmed underwent pretreatment MRI at the Modena facility. MRI was performed using a 1.5-tesla machine between August 2017 and August 2018.
Prior to image acquisition, an antiperistaltic medication was administered intramuscularly to limit bowel peristalsis, and patients were invited to void their bladder to reduce movement and ghosting artifacts on T2-weighted imaging. MR images were acquired with patients lying supine, using a five-channel surface body coil to optimize image quality and reduce acquisition time.
ADC maps were generated on a voxel-by-voxel basis with the software built into the MR unit. The main technique parameters used are shown in the table.
| MRI protocol: Main technique parameters | |||||||
| T2-weighted | T1-weighted | Diffusion-weighted | T1-weighted, multiphase dynamic, contrast-enhanced | ||||
| Sagittal | Axial oblique | Coronal oblique | Axial oblique | Axial oblique | Sagittal | Axial oblique | |
| Pulse sequence | TSE | TSE | TSE | TSE | EPI | GRE | GRE |
| Repetition time (msec) | 5770 | 5000 | 3500 | 708 | 4158 | 4.4 | 4.4 |
| Echo time (msec) | 110 | 120 | 90 | 14 | 66 | 2.1 | 2.1 |
| No. of signals acquired | 2 | 3 | 3 | 3 | 3 | 1 | 1 |
| Section thickness (mm) | 4 | 3 | 3 | 4 | 4.6 | 2 | 2 |
| Section gap (mm) | 1 | 1 | 1 | 1 | 0.3 | -- | -- |
| Matrix | 276 x 221 | 200 x 160 | 232 x 192 | 300 x 150 | 68 x 69 | 112 x 110 | 140 x 160 |
| Field-of-view (mm) | 180 | 160 | 180 | 180 | 180 | 220 | 280 |
Source: Policlinico di Modena, Modena, Italy.
Two radiologists with expert knowledge of gynecologic imaging retrospectively reviewed the MRI scans. The study group had a mean age of 50.04 (± 15.7 years). Squamous cell carcinoma was present in 12 patients, while there was one case each of adenocarcinoma and melanocytic tumor. Eight of the 14 patients were suitable for radical hysterectomy, five underwent chemotherapy, and one was enrolled into another center for surgery. In each patient, the presence or absence of PMI was assessed using T2-weighted imaging and ADC values as predicting tools.
The MRI stage was concordant with the gold standard in 11 of the 13 cases. Five of the 11 patients were correctly staged as IIB (true positive) on the basis of definite parametrium invasion, and six patients were classified as < IIB (true negative) because the hypointense rim sign was clearly intact and it measured about 3 mm. In two patients who had stage IIA disease, MRI findings overestimated the presence of PMI (false positive), probably due to the tumor's large size and to stromal edema; in these cases, it was difficult to assess the intactness of the hypointense stromal ring, which was focally and irregularly thinned.
The results demonstrated that ADC mean values were significantly lower in patients with PMI. The two false-positive patients had higher ADC mean values than those with PMI.
Overall, the study demonstrated that ADC mean values were significantly different in patients with and without PMI, and DWI must be included in the protocol because ADC values improve T2-weighted imaging accuracy in diagnosing PMI in patients with cervical cancer, according to the authors.
The two major limitations of the study are its retrospective nature, which may have resulted in selection bias, and the small number of patients studied. Regardless, the cervical cancer screening program and its high adherence by the female population in Modena could have caused an important reduction of mortality and also allowed tumor detection at an early stage, they concluded.
To view the full e-poster, go to the Modena exhibit in the Electronic Presentation Online System (EPOS) from ECR 2019.