For the first time in almost a decade, the International Federation of Gynecology and Obstetrics (FIGO) has revised the classification system for cervical cancer staging, and it's crucial to be aware of the key amendments, according to expert analysis from the U.K.
"The presence of pelvic and para-aortic nodal disease is now included in the 2018 FIGO staging as a new stage: stage IIIC," noted Dr. M. Salib and colleagues from the radiology department at London's Imperial College Healthcare National Health Service (NHS) Trust. "Stage IIIC is new to the 2018 FIGO classification and is divided into pelvic (stage IIIC1) and para-aortic (IIIC2) lymph node enlargement, again reflecting their importance for treatment planning and prognostication."
Stage IB is now divided into three groups to reflect the prognostic difference in tumors of varying sizes, they added in a digital poster that won a cum laude award at RSNA 2019 in Chicago.
What's to know about cervical cancer?
Cervical cancer is the fourth most common cancer in women of all ages worldwide, and it's the third most common cancer in women younger than 40. Worldwide, it accounts for 7.5% of all female cancer deaths, and some of these deaths could be avoided with adequate diagnosis, staging, and treatment, the authors explained.
Evidence shows that women with tumors smaller than 2 cm in diameter have a twofold increase in survival compared with those with tumors measuring between 2 cm and 4 cm, and therefore the 2009 FIGO stage IB1 has been subdivided into two categories: less than 2 cm, and more than 2 cm but less than 4 cm. Consequently, stage IB2 has been renamed as stage IB3, stated Salib and colleagues.
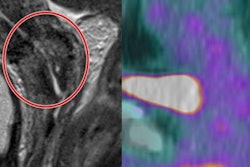
Use of both structural and diffusion-weighted imaging, as well as multiple modalities, including CT and PET/CT, provides a holistic approach to staging in cervical cancer.
In terms of clinical importance, nodal disease on PET/CT is an independent prognostic indicator, they pointed out. Also, the presence and position of nodal metastases affects treatment planning. Studies show that patients with PET-positive nodal metastases had a poorer prognosis than those with similar disease and no nodes.
"PET/CT is used to assess for locally advanced disease in stage IB1 and above tumors as there is increased risk of nodal disease in these patients. This offers greater sensitivity than MRI and CT," the authors wrote.
Disease outside the uterus is metastatic disease and is classified as stage IV. This includes inguinal and supraclavicular lymph nodes, rectal and bladder involvement, peritoneal disease, and pulmonary metastases.
Tumors up to 2 cm in diameter have a lower recurrence rate than those between 2 and 4 cm. Although still treated surgically, the change in staging is used for prognostication.
"Small tumors can be easily missed on a single plane and on morphological imaging alone. It is important to interrogate the structural imaging in multiple planes and correlate with diffusion-weighted imaging," they continued.
Clinical pearls
The Imperial team emphasized that other clinical points to bear in mind are as follows:
- Vaginal involvement is most accurately assessed on clinical examination; there are cases where MRI does not demonstrate vaginal extension, but if there is clear involvement on clinical examination, the patient would be upstaged to 2018 FIGO stage IIA. It is for this reason that all patients undergo an examination under anesthesia prior to surgery.
- Loss of the normal T2 signal intensity of the cervical stroma is the most sensitive imaging finding for parametrial invasion.
- The presence of pelvic nodal disease, regardless of tumor size and location, is now classified as stage IIIC1, according to FIGO. This reflects the significance of nodal metastases, which are an important independent prognostic indicator.
- 2018 FIGO staging now includes nodal involvement, which immediately upstages a tumor to stage IIIC, regardless of the size of the primary lesion and local extension.
- On T2-weighted sagittal imaging, there can be a clear fat plane between the mass and the posterior bladder wall, but on the large field-of-view true axial imaging, partial volume artifact can give the impression of posterior bladder wall involvement. Use of the correct high-resolution, small field-of-view axial oblique imaging, perpendicular to the long axis of the cervix, helps resolve intervening fat planes and confirms that there is no bladder invasion.
- Postbiopsy inflammatory changes can overestimate the size and extension of parametrial invasion. If postbiopsy changes are suspected rather than parametrial invasion, a repeat MRI can be performed after two weeks to confirm resolution. Alternatively, an examination under anesthesia can confirm the presence or absence of parametrial involvement prior to hysterectomy based on the mobility of the cervix.
- A cervical mass larger than 4 cm in diameter is more likely first to extend into the parametrium and then to descend into the vagina rather than extend into the endometrial cavity. Therefore, it is important to consider an endometrial primary and look for a pedicle with a mass of this size and in this location.
- Prolapsed endometrial lesions, such as a carcinosarcoma, can mimic cervical cancer. The pedicle may be of intermediate T2 signal, but in some cases, a prolapsed endometrial polyp will have a vascular pedicle with flow voids, evidenced by a linear low T2 signal pedicle.
In patients with small tumors and a single node, it is important to confirm the disease within the node before upstaging to the inoperable 2018 FIGO stage IIIC1. A frozen section of the lymph node may be necessary to confirm involvement of the node, and the patient should then be referred for chemoradiotherapy. If the node is not involved, the patient would have remained at stage IB1 and undergone a hysterectomy/fertility-sparing treatment and lymphadenectomy, they explained.
Patients who undergo radical trachelectomy do not have an increased risk of recurrence compared to patients with similar disease who undergo hysterectomy. Also, neuroendocrine or clear cell tumors of the cervix are not eligible for surgery, even if they fulfill other criteria; these are fast-growing tumors with poorer prognosis, and therefore chemoradiation is the first-line treatment.
There is an increased risk of late miscarriages in patients who have a radical trachelectomy, the authors noted.