Prizewinning researchers from Spain are convinced that advanced MRI sequences and associated parameters are making rapid progress, and they may play a future role in monitoring the progression and treatment of sarcopenia, an increasingly common disease involving loss of skeletal muscle mass, strength, and function due to aging.
"Efforts should aim at using quantitative and not qualitative information for treatment monitoring, in order to facilitate standardization and the comparison between data from different research groups," noted Drs. Mercedes Vallejo Márquez and Teodoro Martín Noguerol, radiologists in the MRI unit at Health Time in Seville. "Parameters derived from Dixon, diffusion-tensor imaging and T2-mapping acquisitions are quantitative and they show the potential to be considered sarcopenia biomarkers."
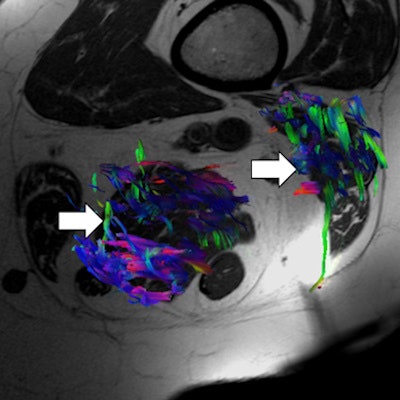
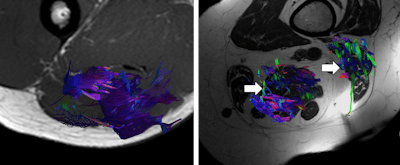 3D reconstructions of muscle fibers of hamstring muscles from diffusion-tensor imaging in a health volunteer (left image) and elderly patient (right image). Note the loss of muscle fiber density in the elderly patient (arrows). All images courtesy of Drs. Mercedes Vallejo Márquez and Teodoro Martín Noguerol.
3D reconstructions of muscle fibers of hamstring muscles from diffusion-tensor imaging in a health volunteer (left image) and elderly patient (right image). Note the loss of muscle fiber density in the elderly patient (arrows). All images courtesy of Drs. Mercedes Vallejo Márquez and Teodoro Martín Noguerol.Sarcopenia is a syndrome characterized by progressive and generalized loss of skeletal muscle mass, strength, and function that occurs as a consequence of aging. It received recognition as a disease entity with the award of an ICD-10-CM (M62.84) code in September 2016 and affects around 5% to 13% of people between 60 and 70 years old and up to half of those older than 80.
"With an aging population that continues to grow, there is an increasing interest in new medical treatments against sarcopenia," they explained in an e-poster presentation that received a cum laude award at RSNA 2018 in Chicago. "The loss of muscle mass in the elderly population is clinically important because it impacts on their normal daily living activities."
Loss of muscle mass also is a strong predictor of mortality. In addition, sarcopenia may have a prognostic role in cancer patients, and there is evidence of the association between sarcopenia, osteoporosis, and hip fracture, the group continued.
What are the diagnostic options?
According to the algorithm proposed by the European Working Group on Sarcopenia in Older People to identify patients with sarcopenia in daily clinical practice, the gait speed of a patient should be measured and compared with the cutoff point of 0.8 m/sec.
If the gait speed is higher than 0.8 m/sec, then the grip strength should be measured. A normal value for grip strength excludes sarcopenia, but a low value for grip strength implies that muscle mass should be measured. If the gait speed is 0.8 m/sec or less, then muscle mass also should be measured. In both situations, the measurement of muscle mass should be performed with a wide range tools, including dual-energy x-ray absorptiometry (DEXA), bioelectrical impedance analysis, CT, MRI, and anthropometry, depending on the local availability and final purpose (research or clinical) of the diagnosis.
Ultrasound can be used in sarcopenia for regional assessment of muscle size and echogenicity, and it is simple and easy to use in clinical practice, particularly in immobile older patients, according to the Spanish authors. Some ultrasound experts suggest that manifestations of sarcopenia appear first in the thigh, particularly involving the quadriceps, before it is visible in the rest of the body. In this early stage, ultrasound may have a role in screening patients before the use of whole-body techniques, they wrote.
CT has proved to be an accurate method in determining body composition using different software that can differentiate tissues in visceral fat, subcutaneous fat, and muscle tissue. The acquisition of a single slice at L3 level is the most common protocol, and some studies show that muscle regional analysis at the L3 level is a strong predictor of whole-body fat and fat-free mass, the authors added.
"CT studies also evaluate the mean attenuation coefficient of muscles. The intramuscular fat infiltration is an important aspect in sarcopenia, which leads to low values of mean attenuation coefficient," they noted. "These low values are directly correlated with increased levels of muscle tissue fatty infiltration and with decreased muscle strength, independently of the muscle cross-sectional area."
Where advanced MRI fits in
Three-dimensional T1-weighted and fluid-sensitive MRI, with or without fat suppression, has a similar role to that of the CT scans in terms of the measurement of the total muscle area and fat-free skeletal muscle area, as concluded after analysis of axial images in different anatomical locations, the researchers stated.
Compared with CT, the main benefits of conventional MRI sequences are the absence of ionizing radiation and a higher contrast resolution for tissue differentiation. Signal alterations in the muscle can be classified into edema, fatty, and mass lesion patterns. Also, MRI can be used to quantify ectopic fat in different organs. The liver, heart, pancreas and skeletal muscles are all considered ectopic fat sites, where fat accumulation can interfere with normal function.
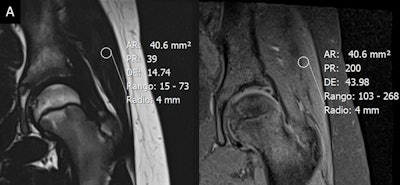 The fat fraction -- measured by a region of interest on the coronal fat- and water-only images from T1-weighted turbo spin-echo Dixon scan of the gluteus medius muscle -- was 16.3% in a healthy 11-year-old patient (A, above) and 36.7% in a 65-year-old patient (B, below).
The fat fraction -- measured by a region of interest on the coronal fat- and water-only images from T1-weighted turbo spin-echo Dixon scan of the gluteus medius muscle -- was 16.3% in a healthy 11-year-old patient (A, above) and 36.7% in a 65-year-old patient (B, below).The Dixon technique is based on the chemical-shift phenomenon and on the principle of separately detecting fat and water protons. Thus, this approach is able to provide fat and water-weighted images for skeletal muscle assessment from a qualitative and quantitative point of view. Whole-body Dixon imaging and quadriceps muscle Dixon imaging have been proposed as markers in sarcopenia.
"Skeletal muscle can be evaluated using diffusion-tensor imaging (DTI) techniques," they wrote. "The role of DTI goes beyond the 3D representation of muscles for evaluation of muscular ruptures or for evaluation of inner fibrillar pattern of each muscular group. The data and parameters derived from DTI acquisition may help to determine the degree of muscular involvement by sarcopenia."
In addition, T2-mapping sequences, previously used for assessing cartilage damage, may be applied for evaluation of fatty infiltration and edema in patients with sarcopenia, they explained.
Pharmacological treatments used in sarcopenia have shown limited efficacy to date, but research and understanding of sarcopenia are important to design new treatments to slow down muscle aging, they concluded.