FDG-PET/CT could be very helpful in calculating the risk of developing interval metastasis during neoadjuvant chemoradiotherapy for esophageal cancer, and it could lead to other more appropriate restaging modalities for patients, according to a study published in the September issue of the European Journal of Nuclear Medicine and Molecular Imaging.
In an analysis of more than 700 consecutive patients, Dutch and U.S. researchers discovered that 8% of subjects developed metastases during treatment and thus avoided a potentially unnecessary esophagectomy because of this routine FDG-PET/CT restaging protocol.
"Accurate preoperative detection of interval metastasis of [esophageal] cancer is crucial for optimal selection of patients suitable for surgery," wrote the researchers, led by Dr. Lucas Goense, from University Medical Center Utrecht in the Netherlands. "In patients with accurately detected interval metastasis, surgery is expected to provide no benefit in terms of survival, but rather to decrease quality of life due to highly morbid surgery with subsequent recovery time."
Treatment debate
It is estimated that more than 450,000 people contract esophageal cancer on an annual basis. In cases of nonmetastasized esophageal cancer, neoadjuvant chemoradiotherapy is the standard of care, while patients with inoperable locally advanced forms of the disease face definitive chemoradiotherapy.
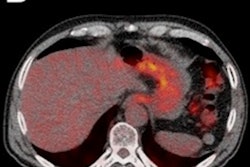
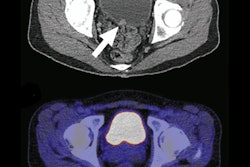
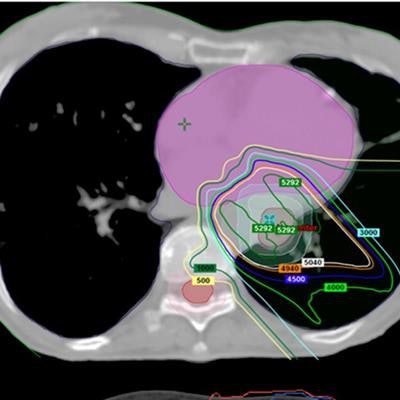
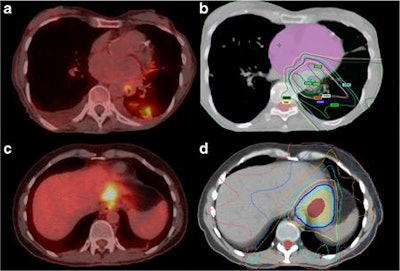 Images show examples of new nonmalignant FDG-avid lesions detected by FDG-PET/CT restaging. A 78-year-old woman (a) with squamous cell carcinoma of the esophagus treated with chemoradiation. PET/CT shows new opacities within the left lower lobe with corresponding areas of FDG activity. The new lesion was within the presumed radiation field (b) and the appearance was most compatible with radiation-induced pneumonitis. Scan was a true-negative for new metastatic disease. A 42-year-old woman (c) undergoing chemoradiotherapy for adenocarcinoma of the distal esophagus. PET/CT shows linear FDG accumulation within the lateral aspect of the left hepatic lobe. A new lesion was within the presumed radiation field (d) and thought to be related to radiation therapy changes. It was a false-positive on MRI, which was required to exclude metastatic disease. Images courtesy of EJNMMI.
Images show examples of new nonmalignant FDG-avid lesions detected by FDG-PET/CT restaging. A 78-year-old woman (a) with squamous cell carcinoma of the esophagus treated with chemoradiation. PET/CT shows new opacities within the left lower lobe with corresponding areas of FDG activity. The new lesion was within the presumed radiation field (b) and the appearance was most compatible with radiation-induced pneumonitis. Scan was a true-negative for new metastatic disease. A 42-year-old woman (c) undergoing chemoradiotherapy for adenocarcinoma of the distal esophagus. PET/CT shows linear FDG accumulation within the lateral aspect of the left hepatic lobe. A new lesion was within the presumed radiation field (d) and thought to be related to radiation therapy changes. It was a false-positive on MRI, which was required to exclude metastatic disease. Images courtesy of EJNMMI."Currently, there is disagreement between guidelines as to whether all patients should be restaged after chemoradiotherapy," the authors wrote. "At present, little is known about which patients are at risk of developing interval metastases."
Thus the objective of this study was to assess FDG-PET/CT's ability to detect and to diagnose interval metastasis and identify predictors of interval metastases in a large cohort of patients with esophageal cancer.
Researchers from University Medical Center Utrecht and University of Texas MD Anderson Cancer Center in Houston, Texas, looked at a total of 783 consecutive patients (mean age, 62.5 years, ± 10.6 years) between 2006 and 2015 who were diagnosed with esophageal cancer. The most predominant tumor type was adenocarcinoma (86%), while the majority of patients (87%) were in clinical tumor stage III (EJNMMI, September 2018, Vol. 45:10, pp 1742-1751).
The subjects underwent an FDG-PET/CT scan (Discovery RX, ST, or STE; GE Healthcare) before and after completion of chemoradiotherapy. After fasting for six hours, patients received between 555 and 740 MBq of FDG.
The mean time between completion of chemoradiotherapy and FDG-PET/CT restaging was 41.3 days (± 10.7 days). After completion of chemoradiotherapy, 450 patients (57%) underwent esophageal resection.
In reviewing the FDG-PET/CT results, Goense and colleagues observed 109 patients (14%) presented with new potential metastatic lesions during restaging. Of these patients, 65 cases were true-positive results (8.3%) confirmed through clinical follow-up (44 patients, 68%) or by histology (21 patients, 32%). By comparison, there were 44 false-positive (5.3%) results.
As the reference standard, the researchers used histological verification or clinical follow-up for diagnostic accuracy measures based on a per-patient basis, and calculated the sensitivity, specificity, and other metrics for PET/CT.
| Accuracy of FDG-PET/CT to detect interval metastasis of esophageal cancer | |
| FDG-PET/CT | |
| Sensitivity | 74.7% |
| Specificity | 93.7% |
| Positive predictive value | 59.6% |
| Negative predictive value | 96.8% |
| Diagnostic accuracy | 91.6% |
In addition, patients with no evidence of interval metastasis after initial restaging with FDG-PET/CT were still at risk of developing new metastatic lesions. The researchers discovered 22 such lesions (50%) among the 44 false-negative results within three months of follow-up.
Because there were no new lesions detected in 86% of patients during restaging after chemoradiotherapy, the authors indicated a "limited impact on patient management is anticipated in the majority of patients .... Consequently, a more individualized application of FDG-PET/CT restaging could reduce the number of unbeneficial diagnostic tests."
On a more somber note, patients with interval metastases had a significantly shorter median overall survival of only six months (range, four to eight months), compared with patients without metastatic disease at restaging who had a mean survival time of with 59 months (47 to 70 months) (p = 0.001).
Predictive score
Goense and colleagues also noted the following independent risk factors for the development of interval metastases:
- Clinical nodal involvement
- Endoscopic ultrasound-based tumor length of 4 cm or more
- Squamous cell tumor histology
- Baseline maximum standard uptake values of 9.6 or greater
"Based on these findings, a prediction score was developed that may provide physicians a tool for objectively assessing the risk of interval metastasis in patients with [esophageal] cancer," the authors wrote. Based on the criteria, a prediction score with an "optimism adjusted C-index of 0.67 demonstrated accurate calibration."
Patients with low predictive scores "have limited risk of interval metastases," the authors wrote, and restaging of these patients based on FDG-PET/CT "may be safely omitted without subjecting the patient to the risks of further diagnostic tests."
The prediction score also "may especially be of interest for hospitals/regions with limited resources that have not yet implemented FDG-PET/CT restaging in their routine clinical practice due to associated costs," the authors advocated.
Because this study was conducted in one facility, Goense and colleagues cautioned that the results may not be applicable to other institutions. "Therefore, external validation of the developed risk prediction score is recommended to determine generalizability," they concluded.