FDG-PET/CT might be considered a double-edged sword when it comes to esophageal cancer. The modality fell short of identifying some higher tumor regression grades, but it detected interval metastases during post-treatment surveillance in a study published in the November issue of the Journal of Nuclear Medicine.
Dutch researchers followed patients who underwent FDG-PET/CT during several phases of their neoadjuvant chemotherapy to evaluate treatment response and look for metastases that might have appeared. Updated disease status is particularly critical after treatment because changes in a patient's condition will directly affect the course of treatment and help determine whether surgery is a more appropriate option.
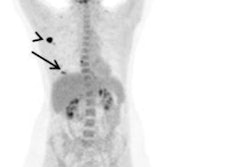
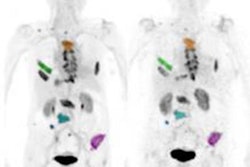
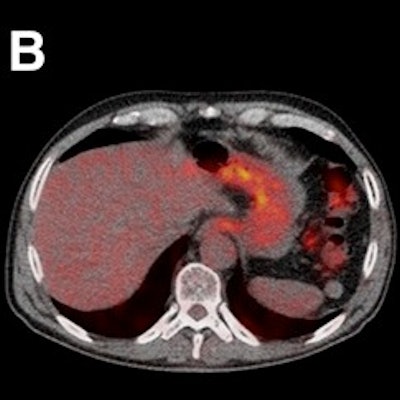
 FDG-PET/CT at baseline (A), 12 weeks (B), and 24 weeks (C) after completion of neoadjuvant chemoradiotherapy. Initial clinically complete response at 12 weeks was followed by an increase in FDG avidity at 24 weeks. In view of these findings, esophagectomy was performed, and residual tumor was found in resection specimen. Resection was radical, and tumor margins were free of disease. Images courtesy of JNM.
FDG-PET/CT at baseline (A), 12 weeks (B), and 24 weeks (C) after completion of neoadjuvant chemoradiotherapy. Initial clinically complete response at 12 weeks was followed by an increase in FDG avidity at 24 weeks. In view of these findings, esophagectomy was performed, and residual tumor was found in resection specimen. Resection was radical, and tumor margins were free of disease. Images courtesy of JNM."It is currently unknown whether it is safe to postpone surgery in patients with a minimal amount of residual tumor," wrote the authors, led by Dr. Maria Valkema from Erasmus University Medical Center in Rotterdam. "We expect that detection of tumor recurrence may be timely -- that is, within the window of opportunity (when complete resection is still possible) -- during systematic rigorous follow-up. However, the duration of this window of opportunity is probably limited."
Long-term survival
Until the introduction of neoadjuvant chemoradiotherapy, patients only had a 35% chance of five-year survival with the disease. Today, long-term survival has increased to 45% to 50% of patients who undergo the treatment, which can induce a compete pathological response in approximately 30% of cases.
"This has raised the question of whether an active surveillance approach can be applied after neoadjuvant chemoradiotherapy," the authors noted. "In such an approach, patients without signs of residual disease after neoadjuvant chemoradiotherapy have regular follow-up clinical investigations. Esophagectomy will be offered only to patients with proven locoregional recurrence, in the absence of distant metastases."
To determine the efficacy of an active surveillance strategy, researchers in the Netherlands created the diagnostic multicenter preSANO trial, which includes data from endoscopies, biopsies, endoscopic ultrasound, and FDG-PET/CT to evaluate patient response to neoadjuvant chemoradiotherapy. Thus, the use of FDG-PET/CT "as a surveillance test is a topic of debate," they added.
For this prospective study, the researchers performed FDG-PET/CT scans at the time of esophageal cancer diagnosis. Four to six weeks after the first round of treatment, FDG-PET scans were conducted again to look for distant metastases in patients with histologically proven residual disease. If there were no metastases, these patients with recurrent disease were scheduled for immediate surgery (JNM, November 2019, Vol. 60:11, pp. 1553-1559).
If endoscopic biopsy results were negative after the first round of chemoradiotherapy, surgery was postponed for another four to six weeks and patients proceeded to a second round of treatment. During this second phase of treatment, FDG-PET/CT again was performed to determine locoregional response and to detect any distant metastases.
Post-treatment evaluations
With the data, the researchers conducted a qualitative analysis that included results from baseline FDG-PET/CT scans and the last imaging exams before surgery. For the quantitative analysis, they manually drew volumes of interest over the primary tumor and visually detected lymph nodes. The same process was performed for the reference regions of the esophagus, liver, and blood pool.
"Our purpose was to prospectively investigate optimal evaluation of qualitative and quantitative F-18 FDG PET/CT in response evaluations 12 to 14 weeks after neoadjuvant chemoradiotherapy in esophageal cancer patients," Valkema and colleagues wrote.
A total of 129 patients were eligible for analyses of their FDG-PET/CT scans after the second round of chemoradiotherapy. Among these patients, FDG-PET/CT could not detect tumor regression grades 3-4 in 18 individuals (15%), resulting in no statistically significant association between the modality and tumor regression grade (p = 0.19). FDG-PET/CT did have a relatively high sensitivity of 80% for detecting tumor regression grades 2-4, compared with tumor regression grade 1, but it achieved specificity of only 37%.
On the other hand, 190 patients were eligible for the analysis of interval metastases detection by FDG-PET/CT. In these cases, the hybrid modality found 38 patients (20%) with a suspicion of distant metastases. In 18 (47%) of those cases, metastases were confirmed as true-positives, while 20 patients (53%) had negative histologic findings and metastases were ruled out after correlation with other imaging and clinical parameters.
"The value of F-18 FDG PET/CT for detection of locoregional recurrence during response evaluation after neoadjuvant chemoradiotherapy for esophageal cancer is limited, both qualitatively and quantitatively," the authors concluded. "Distinction of a small tumor regression grade 3-4 tumor from surrounding physiologic metabolism or postradiation esophagitis is difficult and may lead to false-positive and false-negative results."