Volumetry measurement of lung nodules is gaining clinical acceptance but still poses significant practical difficulties, and major factors of variability are related to the nodule, technical scanner parameters, and hemodynamic issues, according to U.K. researchers.
"Accurate measurement of dimensions/volume of lung nodules is crucial," noted Dr. Diana Penha, a consultant radiologist at Liverpool Heart and Chest Hospital, and colleagues, in an e-poster presented at RSNA 2017. "Before applying volumetry measurements, advise the operator to test and know the software package, especially in the study of smaller nodules."
For nodules with a diameter of more than 8 mm, the variability is related to the method used, and for nodules smaller than 8 mm, variability tends to be much greater, they explained.
Urgent need for accuracy
Obtaining the dimensions of lung nodules is important in daily clinical practice, assessment, follow-up studies of oncological patients, and screening studies for lung cancer, stated Penha, who specializes in in cardiothoracic imaging and chest interventions.
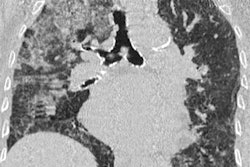
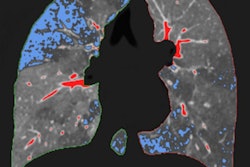
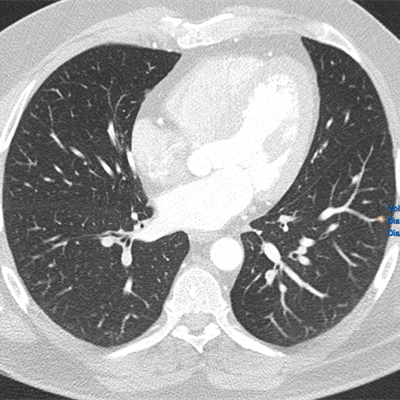
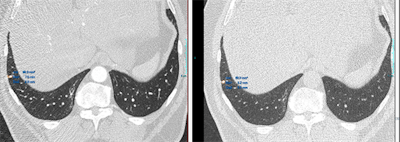 Top images: The semiautomatic lung nodule volumetry tools provides different volume and 2D measurements in different cardiac phases. In the first image, the volume measured is of 89.3 mm3 and in the second, is of 63.3 mm3. All images courtesy of Dr. Diana Penha. Bottom images: The semiautomatic lung nodule volumetry tools provides different volume segmentation that is aberrant in the first image. Due to this aberrant segmentation, the software provided different volumes and 2D measurements.
Top images: The semiautomatic lung nodule volumetry tools provides different volume and 2D measurements in different cardiac phases. In the first image, the volume measured is of 89.3 mm3 and in the second, is of 63.3 mm3. All images courtesy of Dr. Diana Penha. Bottom images: The semiautomatic lung nodule volumetry tools provides different volume segmentation that is aberrant in the first image. Due to this aberrant segmentation, the software provided different volumes and 2D measurements."Nowadays and worldwide we are using 2D measurements/greatest diameter (with electronic calipers), and in the past years, research has been shifting the 2D measurements for 3D volumetry because these are more accurate," she wrote.
Available software provides different types of segmentation modes, tools, and special settings, including manual, semiautomatic and automatic segmentation; measures of volume, 2D/3D diameters, maximum/minimum diameters; histogram; average and standard deviation density; multiplanar reconstruction (MPR); nodule tracking in follow-up studies; dedicated and flexible reporting mode; information saved as DICOM structured reporting data; and report storage and export in different file formats (PDF/HTML).
Factors affecting 3D volumetry consist of those related to the nodule, including its dimensions, location, morphology, and density (solid/ground glass). Various technical parameters are important, particularly slice thickness, software and segmentation algorithms, and inspiratory/expiratory factors. Also relevant here are operator-dependent factors plus interscan, intrascan, and hemodynamic (e.g., cardiac cycle) factors.
"Studies using a 'coffee-break' model showed that different factors such as positioning, inspiratory effort, heart rate, and hemodynamic changes all contributed to interscan variability of nodule's volumetric measurements," the authors stated, adding that inter- and intraoperator variability of less than 1% and interscan variability of 20% can occur. Volume measurement in small nodules can be more than 30% during the cardiac cycle.
The estimated volume of a nodule is based on the number of voxels in the segmented region, while the percentage of voxels with partial volume artifact decreases as the nodules' dimensions increase and the slice thickness decreases. Smaller nodules have a greater percentage of voxels that are affected by partial volume artifact, and volumetric analysis is dependent on the size of the nodule. Furthermore, adjacent location to the airways, vessels, and pleura limits the margin's definition and subsequent segmentation of the nodule.
What the guidelines say
According to the British Thoracic Society's 2015 guidelines for the investigation and management of pulmonary nodules, "Volumetry is recommended as the preferred measurement method and there are recommendations for the management of nodules with extended volume doubling times."
The guidelines recommend considering PET/CT for solid noncalcified nodules > 8 mm or 300 mm3, low-dose CT after one year for nodules of 5 mm to 6 mm, and low-dose CT after three months for nodules of 6 mm to 8 mm or volume 80 mm3 to 300 mm3. The Fleischner Society's 2017 guidelines on management of incidental pulmonary nodules detected on CT also merit close inspection, Penha and colleagues concluded.
Looking to the future, the group is looking to make further improvements to its 3D volumetry technique and to develop 3D printing models for surgeons. "This is my research innovation at the Liverpool Heart and Chest Hospital for 2018," Penha noted.