Using checklists as a guide to interpreting chest CT examinations can help identify diffuse abnormalities in acute disease, according to prizewinning Spanish researchers. If systematically applied, checklists of clinical and radiological data can play a valuable role, they say.
"Differential diagnosis of patients presenting with acute diseases manifesting as diffuse lung disease at chest CT is a diagnostic challenge," noted Dr. Juan Arenas-Jiménez, PhD, and colleagues at the department of radiology, Hospital General Universitario de Alicante. "CT findings alone are usually insufficient to reach a diagnosis, and considering clinical, laboratory, and radiologic factors together help to get a proper diagnosis."
In a digital poster that received a certificate of merit at RSNA 2019, they provided a comprehensive roundup of the most important information to consider when dealing with patients with acute disease and abnormal lungs.
Their aim was to create a reference guide for reading CT with diffuse abnormalities in an acute setting, and they are convinced that if systematically applied, checklists of clinical and radiological data can help radiologists with their diagnosis.
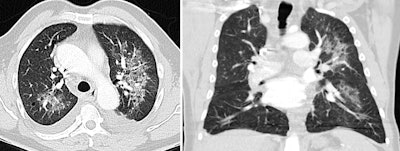 In this case of atypical pulmonary edema, predominant left-sided edema is due to acute mitral valve rupture with eccentric regurgitation seen at echocardiography. Bilateral pleural effusion is also seen. All images courtesy of Dr. Juan Arenas-Jiménez, PhD.
In this case of atypical pulmonary edema, predominant left-sided edema is due to acute mitral valve rupture with eccentric regurgitation seen at echocardiography. Bilateral pleural effusion is also seen. All images courtesy of Dr. Juan Arenas-Jiménez, PhD.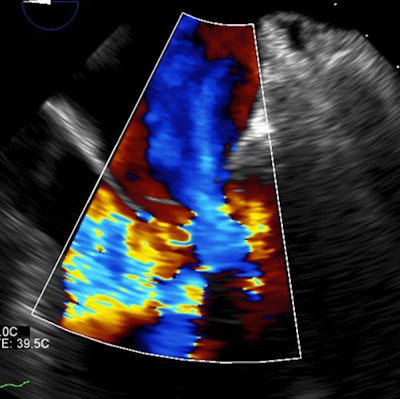
In many of these cases, the clinical symptoms are unspecific, though in patients with diffuse abnormalities of the lungs, dyspnea should almost always be present, according to the authors. Some pivotal findings provide valuable information about the clinical problem in a given patient, including the following:
- Fever: Fever is usually considered a sign of infection, but it can be a confounding factor because it is present in many noninfectious diseases. Be reluctant to diagnose infection only on the basis of the fever, they stated.
- Orthopnea: This is a cardinal symptom of heart failure.
- Hemoptysis: In an appropriate clinical setting -- and along with conditions associated with diffuse alveolar hemorrhage, such as vasculitis, connective tissue diseases, and hematological abnormalities -- hemoptysis supports the diagnosis.
"Although hemoptysis is a cardinal sign of diffuse alveolar hemorrhage in a patient with bilateral pulmonary opacities, it must be kept in mind that it may be absent in up to one-third of patients. On the other hand, blood-tinged sputum isn't rare in pulmonary edema, and hemoptysis can appear in infections and acute respiratory syndrome," they explained. - Cutaneous lesions: A range of cutaneous lesions can elucidate the diagnosis, such as petechial rash in fat embolism.
- Hematuria: Hematuria associated with acute lung disease should prompt the diagnosis of pulmonary-renal syndromes. Proteinuria, autoantibody determination, and blood in a bronchoalveolar lavage support the diagnosis.
- Vomiting: Vomiting can be the main symptom associated with aspiration of either oropharyngeal material or gastric contents, although underlying loss of consciousness usually increases the risk.
"Some diseases are linked to specific lung complications that can have a typical clinical-radiologic presentation. We must always think about them," the authors wrote.
The relevant laboratory tests in these cases are white blood cell counts (low/high/0, lymphopenia, eosinophilia) and checks for anemia (recent onset?), low platelets, D-dimer, N-terminal pro b-type natriuretic peptide (NT-proBNP), renal function, and urinalysis.
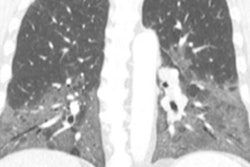
 An 89-year-old woman presented with dyspnea and elevated D-dimer. Cardiomegaly and marked elevated proBNP suggested the diagnosis of unilateral pulmonary edema that resolved after diuretic treatment. D-dimer levels are elevated in most patients with acute thrombosis, but the levels also are increased in advanced age, after surgery, during pregnancy and puerperium, with cancer and other chronic inflammatory conditions, and in many other disorders. D-dimer elevation is the cause of request for many CT angiograms that finally reveal an alternative diagnosis causing dyspnea.
An 89-year-old woman presented with dyspnea and elevated D-dimer. Cardiomegaly and marked elevated proBNP suggested the diagnosis of unilateral pulmonary edema that resolved after diuretic treatment. D-dimer levels are elevated in most patients with acute thrombosis, but the levels also are increased in advanced age, after surgery, during pregnancy and puerperium, with cancer and other chronic inflammatory conditions, and in many other disorders. D-dimer elevation is the cause of request for many CT angiograms that finally reveal an alternative diagnosis causing dyspnea.On drug toxicity, the group suggests always bearing in mind treatment-related reactions, especially in patients with neoplasms, connective tissue, and transfusions. These reactions can appear in recently initiated or long-standing treatments.
System checklist
Many primary pulmonary conditions can show an acute presentation or exhibit acute complications. These patients often present at the emergency department, but their conditions are the result of a progressive subacute disease. Infection should be considered as a differential diagnosis in most patients.
The specific system checklist given by Arenas-Jiménez and colleagues comprises the following:
- Pulmonary: Broad category, interstitial lung diseases, eosinophilic lung diseases, inhalational, lung cancer
- Neurologic: Low consciousness, neurogenic pulmonary edema, treatment with corticosteroids, fat embolism
- Cardiac: Known heart disease, valvulopathy, amiodarone
- Gastrointestinal: Vomiting, transfusion, long-term treatments, neoplasms
- Urologic: Hematuria in pulmonary-renal syndrome, infection and sepsis (acute respiratory distress syndrome), treatments
- Connective: Interstitial lung involvement by the disease, treatment related, infections
- Hematologic: Fluid overload, infections, neoplasms, granulomatous-lymphocytic interstitial lung disease, syndrome differentiation, bone marrow transplant
- Oncologic: Therapy related (chemotherapy, radiotherapy), infections, tumoral progression
Be sure to check for previous examinations, they recommended. Chest x-ray abnormalities showing a few hours of onset are typical in pulmonary hemorrhage, cardiogenic edema, transfusion-related acute lung injury, and aspiration. Also, check for previous cardiac size, and look for signs of fibrosis in previous examinations as a clue to acute exacerbation of fibrosis.
"Check for a typical pattern," the authors advised. "The presence of typical chest CT patterns can make the diagnosis straightforward, however they gain specificity when presenting in a characteristic clinical background. The main abnormalities, their distribution, and ancillary findings confirm the specific patterns."
Many of the conditions are not really urgent situations; they are subacute or progressive diseases. Patients often present at the emergency department for dyspnea, requiring a diagnostic approximation, and appropriately orienting those patients is desirable, they added.
In their analysis, the investigators decided to exclude all traumatic injuries, vascular conditions such as pulmonary embolism, the detailed discussion of characteristics of pulmonary infections, and specific situations like pulmonary lung disease in solid organ transplants and severely immunosuppressed hematologic patients who have a distinct, more complex differential diagnosis.