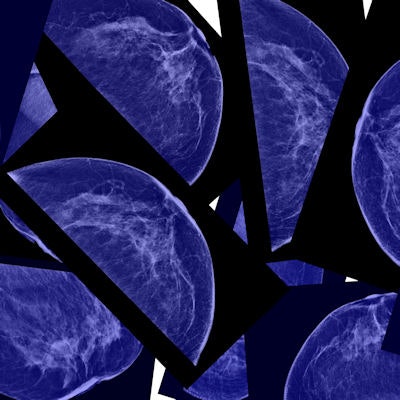
A new Danish study shows breast cancer screening in the country performs well, with a sensitivity of more than 70% and a specificity of nearly 98%. The researchers also refute claims from other studies that question whether pilot screening programs reduced breast cancer mortality and only led to overdiagnosis.
The study team, led by Elsebeth Lynge, a professor of occupational and environmental health at the University of Copenhagen, looked at the short-term outcomes of the national Danish screening program to determine its effectiveness. She and her colleagues also addressed the confusion surrounding the effect of pilot programs claiming the pilots caused more harm than benefit. To characterize the programs in such a way is to misunderstand them, according to Lynge and colleagues.
"Our study showed that even within the small Danish population the variations in both screen detection and false-positive rates were surprisingly large, but all regions are working quite well in accordance with European and national guidelines," they wrote (BMC Cancer, 28 December 2017). "Screening mammography is a delicate balance between benefits and harms, and the Danish experiences illustrate the importance of close monitoring of short-term quality indicators."
National performance
Denmark started regional breast screening programs in the early 1990s and implemented a national rollout in 2007 to 2010. The success of the regional programs in reducing breast cancer mortality has been the subject of heated debate; in particular, researchers from the Nordic Cochrane Center have charged that the pilot programs have not reduced breast cancer mortality and have only led to overdiagnosis.
While it's still too early to assess the impact of the national program on mortality, it is possible to review short-term indicators for signs of its success, such as interval cancer rate and rate of screen-detected cancers, which could correlate well with the later decline in breast cancer mortality, the authors noted. So Lynge and colleagues focused on these short-term indicators to see if the program was on the right track.
They retrieved data from the 2015 and 2016 national screening quality reports and calculated coverage by examination (the number of screened women divided by the target population); participation after invitation; rates of cancer detection, interval cancers, and false positives; cancer characteristics; sensitivity; and specificity for Denmark nationally and for the five regions.
They found three-quarters of Danish women participated in the screening mammography program. In terms of specific cancers, slightly less than 1% of women had invasive carcinoma or ductal carcinoma in situ (DCIS) detected during their first screen and around 0.6% in subsequent screens.
The proportion of women with DCIS remained constant: 13% to 14% during the four invitation rounds. In subsequent rounds, 75% to 80% of screen-detected invasive breast cancers were lymph node-negative and 40% had a diameter of 10 mm or smaller.
"The screening program thus detected mainly invasive, lymph node-negative breast cancers with a high proportion of small cancers," the authors wrote.
Results are summarized in the table below.
| Performance of national screening mammography in Denmark | ||||
| 1st round 2008-2009 (%) | 2nd round 2010-2011 (%) | 3rd round 2012-2013 (%) | 4th round 2014-2015 (%) | |
| Coverage of exam | 75.4 | 75 | 76.7 | 76.4 |
| Participation after invitation | 76.4 | 81.8 | 84.3 | 82.1 |
| Detection rate | 0.93 | 0.62 | 0.67 | 0.61 |
| False-positive rate | 2.04 | 2.08 | 2.07 | 1.88 |
| Invasive | 87.5 | 86.3 | 86.4 | 85.8 |
| DCIS | 12.6 | 13.7 | 13.6 | 14.2 |
| Interval cancer rate | 17.9 | 28.9 | 26.3 | N/A |
| Sensitivity | 82.1 | 71.2 | 73.7 | N/A |
| Specificity | 97.9 | 97.9 | 97.9 | N/A |
Cochrane controversy
Denmark initiated two pilot programs in the 1990s, which constituted almost a "natural experiment" of breast cancer screening. Using individually linked cohort data from one pilot in Copenhagen, Anne Helen Olsen et al found breast cancer mortality in Copenhagen decreased by 25% more than expected in the absence of screening (BMJ, 29 January 2005, Vol. 330:7485, pp. 220). In the other pilot program in Funen, Sisse Helle Njor et al found a decrease of 22% (Journal of Medical Screening, March 2015, Vol. 22:1, pp. 20-27).
However, in the 2017 Cochrane study by Dr. Karsten Juhl Jørgensen et al, the researchers used routine breast cancer mortality data from fixed age groups to conclude they were unable to detect any effect of the Danish screening programs on breast cancer mortality. Why did results from the Cochrane study conflict with those from the previous two studies?
Jørgensen and colleagues included breast cancer deaths from women diagnosed with breast cancer prior to the start of the screening program, and these women had no chance to benefit from screening, according to Lynge and colleagues. However, Olsen et al used incidence-based mortality including only deaths from breast cancer in women diagnosed after the start of the screening program, and thus those who had a chance to benefit from screening. Also, Jørgensen et al only looked only at average annual change in the trends of breast cancer mortality before and after the start of screening.
"They left out observations from the first seven years after start of the screening programs, and thus ignored changes in breast cancer mortality during this period," Lynge and colleagues wrote. "In fact, a recalculation of the data reported by Jørgensen et al showed a decline of 13% in breast cancer mortality in the screening areas as compared with the decline in the nonscreening areas. Given that the Jørgensen et al data were contaminated with breast cancer deaths in women diagnosed prior to screening, this 13% decline is fairly much in line with the 22% to 25% decline observed by Olsen et al and Njor et al in the noncontaminated data."
Similarly, in terms of overdiagnosis, using individually linked data from cohorts of women offered screening and followed for a minimum of eight years after the end of screening age, the overdiagnosis numbers are different: 2.3% versus 33%.
"Screening introduces a dynamic in the incidence of breast cancer with a prevalence peak, an artificial aging, and a compensatory dip," the authors wrote. "This dynamic is captured correctly only by following the cohorts of screened women."
Jørgensen and colleagues did not capture the compensatory dip and inflated their estimate of overdiagnosis by geographical differences in breast cancer incidence prior to the introduction of screening, according to Lynge and colleagues.
Regional differences
For the current study, Lynge and colleagues spotted some regional differences. As in other urban settings, the coverage was relatively low in the Capital Region, particularly in the second round, where the coverage was 68% in the Capital Region compared with the national average of 75%.
"The second round coincided with the publication of a study that claimed screening lead to heavy overdiagnosis, and that one-third of breasts were removed without reason," the authors wrote. "Women in the Capital Region may have been more sensitive than other women to negative messages reported in the media. It is noteworthy that coverage in the Capital Region in the third and fourth rounds were back to the higher level from the first round."
In Region Zealand, the detection rate fluctuated over time in contrast with other regions. The researchers identified a low detection rate of 0.53% in the third round, while the national average was 0.61%, possibly because the prevalent pool of breast cancers was depleted at that time.
"This should then have been followed by a high sensitivity, which was not the case," the authors wrote. "The region has suffered from shortage of experienced radiologists. It remains to be seen what the sensitivity will be in Region Zealand after the fourth round."
Despite the differences, the researchers concluded the breast cancer screening program is effective.



















