Given its high sensitivity and negative predictive value, French researchers are promoting FDG-PET/CT for its ability to assess response to treatment and redirect therapy for patients with recurrent or progressive anal cancer, in a study published in the September issue of the Journal of Nuclear Medicine.
Using FDG uptake from FDG-PET/CT scans as an indication of metabolic response to chemoradiotherapy, radiologists were able to predict two-year progression-free survival. In cases of cancer recurrence, they were able to direct patients toward surgery (JNM, September 2017, Vol. 58:9, pp. 1414-1420).
"FDG-PET/CT has good accuracy in the post-treatment evaluation of anal cancer and has a beneficial impact on patient care. Moreover, complete metabolic response was associated with good survival outcome," wrote the researchers, led by Dr. Clémence Houard from Centre Hospitalier Universitaire de Bordeaux. "Taken together, FDG-PET/CT may become an important asset for post-treatment follow-up of anal cancer."
Increasing cases
While anal carcinoma has a relatively low worldwide incidence rate of 1 in 100,000 people, the number of cases has been growing in developed countries in recent decades, particularly among younger homosexual men and individuals with immunodeficiency, such as transplant recipients and those with AIDS, the authors noted.
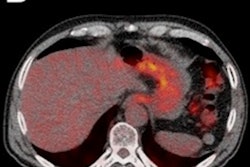
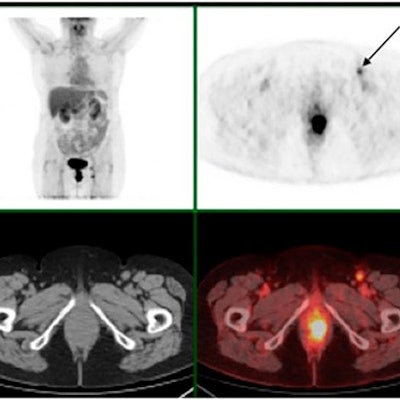
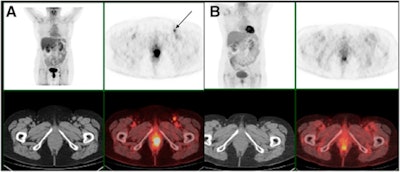 FDG-PET/CT before treatment (A) shows an anal tumor on axial slices and a left inguinal node (black arrow). FDG-PET/CT four months after chemoradiotherapy (B) shows persistent increased FDG uptake in anal canal (noncomplete metabolic response) but complete regression of inguinal node uptake. Persistent disease was proved by biopsy. Images courtesy of JNM.
FDG-PET/CT before treatment (A) shows an anal tumor on axial slices and a left inguinal node (black arrow). FDG-PET/CT four months after chemoradiotherapy (B) shows persistent increased FDG uptake in anal canal (noncomplete metabolic response) but complete regression of inguinal node uptake. Persistent disease was proved by biopsy. Images courtesy of JNM.Patients are most often treated with radiotherapy and chemotherapy, with a five-year disease-free survival rate of 67%, they wrote. For patients with disease recurrence or progression, surgery is the most common course of action.
The challenge for physicians is evaluating the response to treatment. Edema, residual fibrosis, and scar tissue can obscure recurrent anal cancer in ultrasound, MRI, and CT scans. The National Comprehensive Cancer Network recommends FDG-PET/CT for the initial diagnosis and staging of primary disease, but only a handful of studies have explored its efficacy for anal cancer patients, and those papers have included small patient samples.
This multicenter retrospective study from France included 87 anal cancer patients with a median age of 62 years (range, 35-89 years). Among the 68 women and 19 men, 43 patients (49%) had a T1 or T2 tumor and 44 (51%) had a T3 or T4 tumor. Thirty-eight patients (44%) were staged as N0, 50 (57%) were N+, and five (6%) had liver metastases.
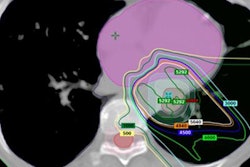
Pretreatment staging included a physical exam, CT, rectal endosonography, pelvic MRI, and FDG-PET/CT before chemoradiotherapy between October 2007 and October 2013. Follow-up included FDG-PET/CT (Discovery 690, GE Healthcare, or Gemini TOF 16, Philips Healthcare) at one of three nuclear medicine departments.
Treatment follow-up
The median follow-up after treatment began was 25 months (range, 8-76.9 months). No patient had a follow-up time of less than six months. A total of 62 patients (71%) had no evidence of recurrence at the end of follow-up.
Based on the FDG-PET/CT results, 55 patients (63%) experienced a complete metabolic response to treatment, which was defined as having no abnormal FDG uptake. Thirty-two patients (27%) had abnormal FDG uptake and were considered to have an incomplete response to treatment. Among the latter set of patients, 17 (53%) showed disease progression, while 15 (47%) had a partial metabolic response.
The two-year progression-free survival rate was 96% for patients with a complete metabolic response, compared with 28% for patients with a poor metabolic response to treatment (p < 0.0001). The researchers also evaluated cause-specific survival (CSS), which was defined as the period from treatment initiation to the date of death due to anal cancer. The two-year CSS rate was 100% for patients with a complete metabolic response and only 59% for patients without a complete metabolic response (p < 0.0001).
The researchers concluded that a complete metabolic response with no abnormal FDG uptake was the only significant predictor of progression-free survival and cause-specific survival. Conversely, initial staging for tumors or nodes was not significantly associated with progression-free survival and cause-specific survival.
Care management
FDG-PET/CT changed treatment management in 14 cases (16%), which included eight cases of previously unseen local recurrences. The results were confirmed by biopsy and led to salvage surgery for the patients. In addition, one patient avoided an unnecessary biopsy, despite an inconclusive clinical examination and a positive MRI.
The researchers also found that FDG-PET/CT's high sensitivity and high negative predictive value tracked findings in previous studies.
| FDG-PET/CT for detecting residual tumor | |||||
| Sensitivity | 92% | ||||
| Specificity | 85% | ||||
| Positive predictive value | 72% | ||||
| Negative predictive value | 96% | ||||
"This high negative predictive value may prevent unnecessary biopsies or surgery for patients with postradiotherapy modifications, which is particularly clinically relevant because biopsies are associated with a significant risk of necrosis," Houard and colleagues wrote.
The group noted several limitations of the study, including its retrospective approach, which could result in some heterogeneity regarding treatments, FDG-PET/CT protocols, and referral strategies. To minimize heterogeneity, two experienced nuclear medicine physicians reviewed all FDG-PET/CT images with no knowledge of clinical results.