
Lung nodule assessment software can be used to accurately differentiate histological subtypes of lung adenocarcinomas manifesting as ground-glass nodules, helping to reduce diagnostic uncertainty in managing these common lesions, according to Austrian research published online by European Radiology.
A team led by Dr. Ursula Nemec of the Medical University of Vienna and Dr. Benedikt Heidinger of Beth Israel Deaconess Medical Center in Boston used the Computer Aided Nodule Assessment and Risk Yield (CANARY) software developed at the Mayo Clinic in the U.S. to evaluate over 60 pure ground-glass nodules. They found significant differences in risk components between the three histological subtypes of these adenocarcinomas. What's more, a threshold of 45% or less of low-risk components in the nodule yielded 100% specificity and 100% positive predictive value (PPV) for invasive tumors.
"While the precise role of CANARY in the workup of [adenocarcinomas] remains to be determined, our study suggests a potential role for this software in suspected adenocarcinomas manifesting as pure ground-glass nodules on CT, notably for patients with high risk of invasiveness," the authors wrote.
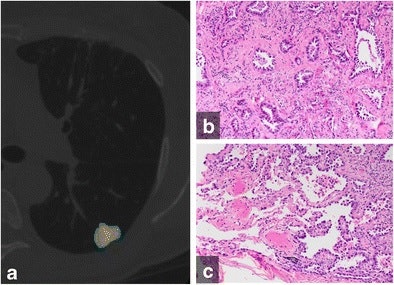 (A) Color-coded CANARY output overlay of invasive adenocarcinoma (yellow-pink-cyan). Cyan represents low-risk components, while pink and yellow indicate intermediate-risk components. The software found the nodule included 32% low-risk components, 66.9% intermediate-risk components, and 1% high-risk components. (B) Histologic image from the central area of the tumor shows the invasive acinar growth pattern (C) Histologic image from the tumor periphery showing noninvasive lepidic growth pattern and adjacent uninvolved lung parenchyma (H&E stain, 200x original magnification). Images courtesy of European Radiology.
(A) Color-coded CANARY output overlay of invasive adenocarcinoma (yellow-pink-cyan). Cyan represents low-risk components, while pink and yellow indicate intermediate-risk components. The software found the nodule included 32% low-risk components, 66.9% intermediate-risk components, and 1% high-risk components. (B) Histologic image from the central area of the tumor shows the invasive acinar growth pattern (C) Histologic image from the tumor periphery showing noninvasive lepidic growth pattern and adjacent uninvolved lung parenchyma (H&E stain, 200x original magnification). Images courtesy of European Radiology.CANARY software
The CANARY software package was designed to identify pulmonary nodules that are aggressive and potentially cancerous from those that are not aggressive and potentially could be treated with less extensive surgery. It assesses voxel densities of pulmonary nodules on high-resolution CT scans and then categorizes risk based on voxel proportion and clustering. Voxel densities are classified as having low-, intermediate-, or high-risk components, each of which are color-coded as an overlay on the image.
The software can noninvasively stratify the risk that lung adenocarcinomas can pose by characterizing the nodule as noninvasive adenocarcinoma in situ (AIS), or invasive subtypes such as minimally invasive adenocarcinoma (MIA) or invasive adenocarcinoma (IAC). While CANARY has been shown to be accurate in assessing the histology and outcome in a morphologically diverse number of lung adenocarcinomas, it has not yet been tested in lung adenocarcinomas manifesting as pure ground-glass nodules, which have a morphologically more uniform appearance on CT.
"A tool to differentiate among these histological subtypes in lung adenocarcinomas could help to reduce diagnostic uncertainty in the management of such nodules," the authors wrote.
As a result, the researchers sought to evaluate the performance of CANARY in differentiating and assessing risk for these pure ground glass nodules (Eur Radiol, 14 July 2017).
The group used CANARY to retrospectively assess 64 biopsy-proven pure ground-glass nodules from 59 patients. Of these, 28 (44%) were AIS, 26 were MIA, and 10 (16%) were IAC. The nodules had an average diameter of 14.4 ± 5.3 mm on CT.
Significant differences
CANARY found statistically significant differences in risk components between the histological subtypes (p < 0.001 to 0.003), according to the researchers.
"Our study showed that in [adenocarcinomas] manifesting as pure ground-glass nodules on CT, CANARY software allowed the differentiation of the histological subtypes AIS, MIA, and IAC," the authors wrote.
While previously published studies had also found differences in risk components between histological subtypes of adenocarcinomas, those studies included morphologically heterogeneous groups of adenocarcinomas, according to the group.
"Therefore, to the best of our knowledge, our findings are novel in showing these differences in a homogenous group by exclusively including only [adenocarcinomas] manifesting as pure ground-glass nodules," the authors wrote. "This is important because risk assessment of [adenocarcinomas] manifesting as pure ground-glass nodules is essential for choosing a management approach such as CT follow-up interval, time of biopsy, and selection of an appropriate surgical method."
The researchers also determined that a 45% or less relative volume of low-risk components in the nodule -- as determined by the CANARY software -- reflected histological invasiveness. That threshold yielded 100% specificity and 100% PPV.
On the downside, CANARY only produced 30% sensitivity for histological invasiveness. However, a previously published pilot study had reported sensitivity of 95.4% to 98.7% and a negative predictive value of 87.5% to 96.8% for a different histological subcategorization of pulmonary adenocarcinomas, according to the group.
"Therefore, and because this study also included both, solid and part-solid lesions, the diagnostic performance of these two studies are difficult to compare," they wrote.
The authors also noted they believe the analysis software offers a better means than just considering lesion size for predicting the invasiveness of adenocarcinomas.
"This prediction is important as patients with suspected invasive nodules are more likely to undergo more follow-up examinations, earlier biopsies, and more radical surgical resections," they wrote. "In particular, the software may be used in high-risk patients."



















