Harnessing the power of new technology can enable more clinical teams to acquire and print 3D models from the pelvis and hip, making use of existing, up-to-date, preoperative, cross-sectional imaging and leading to substantial cost savings, according to research presented at the 2017 meeting of the European Society of Musculoskeletal Radiology (ESSR).
Appreciation of the residual bony anatomy, bone loss, displacement of the surrounding soft tissues, and the 3D spatial relationships between all four is critical to surgical planning, according to Dr. Danoob Dalili, a specialist registrar for clinical radiology and research fellow at Guy's and St. Thomas' National Health Service (NHS) Foundation Trust, and colleagues.
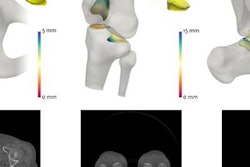
"Three-dimensional printing, when married with medical imaging, allows the reproduction of anatomy in a patient-specific model, thus capturing the radiologist's expert understanding of the CT scan within an immediately accessible, tactile form, which the surgeon can hold in their hands," they noted in an e-poster presented at the annual meeting of the ESSR, held in mid-June in Bari, Italy. "These models represent a true size of the patient's anatomy and are made to scale. They can be produced quickly and allow for enhanced visualization and physical interaction."
The configuration of the patient's hip joint often is distorted due to mechanical failure, the reaction at the interface between bone and the primary prosthesis, underlying osteoporosis, and hardware failure over time, explained the researchers, whose hospital is a tertiary referral center for patients with complex hip pathology and is one of the U.K.'s largest specialist young adult hip units.
The models are of great benefit for technically challenging cases, such as when there is anatomic variance, complex fracture patterns, or in revision reconstruction, they continued. The ability to hold a scale model allows for the simulation and then practice of the surgical technique, simulating the procedure and investigating the use of a range of solutions prior to entering the operating room.
The Guy's and St. Thomas' hip research group is led by consultant musculoskeletal radiologist Dr. Amanda Isaac.
Facts about complex cases
In 2012, over 80,000 total hip replacements (THRs) were performed in the U.K., according to Arthritis UK. More than 1 in 10 of the THRs (about 8,600) were revision THRs, and there is evidence the number of revision THRs performed is increasing.
Because all cases are different, the exact time taken depends on the complexity of the individual case, but in general it takes at least twice as long to do a revision THR as it does to do a first-time THR. Thus it takes a minimum of two to three hours, and significantly longer in more complex cases, and it is specialist surgery requiring the use of specialist techniques and specialist equipment, Arthritis UK noted.
Against this background, Dalili and colleagues decided to assess the value of 3D models of the hip joint in surgical care, utilizing current preoperative cross-sectional imaging modalities. They conducted what they think is the first study investigating the added value of 3D printing technology in complex THRs, and they are convinced this approach enhances surgical care preplanning, and has a potential effect on both short-term and long-term patient outcomes and health economics.
They prospectively collected preoperative CT data from 10 patients listed for complex revision hip arthroplasty (CRHA) and digitally reconstructed images using 3D printing software. All revision cases were discussed amongst three experienced hip surgeons and a musculoskeletal radiologist, who were asked to complete a short written questionnaire.
The level of complexity of the cases was ascertained by consensus among the surgeons. Thereafter, they were presented with the 3D model and asked to repeat the process and complete a written questionnaire about the proposed surgery, proposed prosthesis and size(s), expected operative time, expected recovery time, and degree of confidence in the details of proposed procedure, using a visual analog score (calibrated 0 to 10).
For independent record keeping, the physician associate recorded the details of the surgery, cost of the prosthesis, total operative savings, length of hospital stay, and rehabilitation (from the physiotherapists' formal notes).
"Our study was low-risk, as it utilized existing preoperative imaging, with no added radiation exposure," the authors wrote. "All cases were discussed in a multidisciplinary setup and a consensus amongst experienced surgeons was obtained prior to surgery. The surgeons used standard complex THR implants. There were no changes to the anesthetic protocols routinely used. There were no changes to the rehabilitation protocol initiated and led by our physiotherapists, who were blinded to the study."
What were the cost benefits?
In a fairly typical case, the surgical time was 4 hours and 3 minutes, the anesthetic time was 5 hours and 33 minutes, and the intraoperative blood loss was less than 500 mL (hemoglobin preoperative 133 and 98 postoperative, no blood transfusion required postprocedure). The hospital stay was five days, and the prosthesis (TMARS implant by Zimmer) cost 4,000 pounds, or around 4,476 euros. The loan kit cost was between 200 pounds and 600 pounds (224 euros and 672 euros). The cost of the 3D model was 748 pounds (837 euros).
The total savings using 3D printing were estimated to be more than 2,000 pounds (2,240 euros). An alternative to this 3D model was to use a custom-made implant, costing between 12,000 pounds and 16,000 pounds (13,430 euros and 17,900 euros), instead of the "off-the-shelf TMARS implant."
The pilot study had the following important advantages:
- Shortened the operative time by 30 to 90 minutes, reducing the cost of surgical and other medical staff time, allowing more procedures to be performed on the day and thus reducing waiting lists.
- Reduced the excess of preordered prostheses, lowering shelf-kit loan costs and overall operative costs.
- Subjectively improved patient outcomes through reduced anesthetic time, intraoperative manipulations with associated blood loss, and soft-tissue bruising.
- Improved the surgeon's confidence in preoperative planning through the choice of appropriate prosthesis, position, and trajectory for screw placement.
- Allowed for "elective" peer review discussion of the case in a multidisciplinary team meeting. Traditionally, decisions can only be made intraoperatively, once the old implant is removed, as the acetabular bed is prepared and the extent of bone loss and residual bony configuration is established.
Overall, the group said its findings confirm a positive effect on costs, operating room flow, and patients' stay in hospital, thereby having an effect on the total number of complex THRs performed per year and shortening the waiting lists for surgery. Furthermore, this may contribute to overall improved quality of life in this particular cohort of patients.
Now a more robust prospective research study is underway by the hip research group, the researchers concluded. The research has been entirely designed, conducted, financed and printed exclusively in the Guy's and St Thomas' Trust, and the hip research group is based in the trust.
For free access to the authors' full range of clinical cases and images presented at ESSR 2017 and available on the European Society of Radiology's EPOS database, click here.