Adding a technique called mechanical imaging to mammography breast cancer screening could lower the number of false positives and recalls by a third, according to a new Swedish study. The researchers call the results "surprising."
Mechanical imaging is the practice of deforming tissue and measuring the resulting distribution of pressure, or stress field, using pressure sensors. There are differences in the mechanical properties of various types of breast tissue -- the elasticity modulus relates the stress (pressure exerted on the material) to the strain (relative deformation of the material), explained lead author Magnus Dustler, a medical radiation physics doctoral student at Lund University in Malmö, Sweden. That means the greater the elastic modulus, the stiffer the material.
In the study, women recalled from a breast screening center had mechanical imaging readings acquired of the symptomatic breast to determine if mechanical imaging could differentiate malignant lesions from benign ones. The team found adding mechanical imaging could reduce biopsy and recall rates by as much as one-third (European Radiology, 20 January 2017).
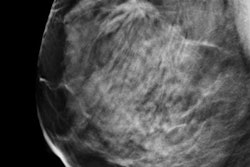
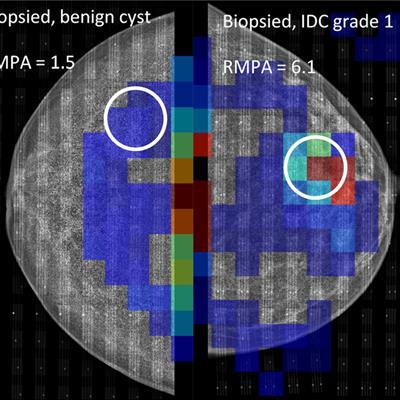
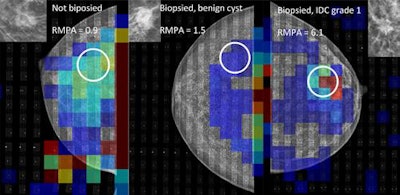 Examples of mechanical imaging data from the study, matched with corresponding mammogram. All three groups are represented, from left to right: A, not biopsied, presumed benign; B, biopsied, benign; and C, biopsied, malignant. Note the presence of a high-pressure area outside of the breast on the left-most image; it is caused by wrinkling of the sensor. This is one example of a technical problem, which in this case did not affect the measurement. All images courtesy of Magnus Dustler.
Examples of mechanical imaging data from the study, matched with corresponding mammogram. All three groups are represented, from left to right: A, not biopsied, presumed benign; B, biopsied, benign; and C, biopsied, malignant. Note the presence of a high-pressure area outside of the breast on the left-most image; it is caused by wrinkling of the sensor. This is one example of a technical problem, which in this case did not affect the measurement. All images courtesy of Magnus Dustler."The results were surprising in a good way," Dustler told AuntMinnieEurope.com. "We thought that we might be able to find something, but we were not expecting such a large difference between malignant and benign lesions."
There is a considerable difference in elastic modulus between various types of benign and malignant breast tissue, so mechanical imaging may be used to differentiate such structures, the authors continued. Malignant tumors have a substantially greater elastic modulus than other tissues, especially at higher degrees of deformation (strain).
"The tissues in the human breast are nonlinearly elastic, which means that the value of the elastic modulus increases with the level of strain," the authors stated.
In earlier studies, Dustler and colleagues used a Tekscan Iscan force-sensing resistor system consisting of pressure sensors attached to the compression plate of a mammography device to obtain pressure readings of the compressed breast. In the new study, they affixed two Iscan model 9801 sensors to the inferior side of the compression paddle of a Mammomat Inspiration mammography system (Siemens Healthineers). Each sensor consists of 96 individual sensor elements, arrayed in six rows of 16. Each sensor element is a square with a side of 12.7 mm and a total thickness of roughly 0.16 mm.
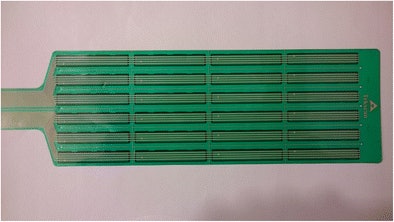 A Tekscan Iscan 9801 pressure sensor employed in the study. Each strip consists of four sensor elements. The electrical impedance of the sensor elements decreases when subject to pressure.
A Tekscan Iscan 9801 pressure sensor employed in the study. Each strip consists of four sensor elements. The electrical impedance of the sensor elements decreases when subject to pressure.The use of pressure sensors during mammography screening, giving real-time pressure reading in conjunction with the screening images, has not previously been investigated -- until now.
"We hypothesized that mechanical imaging could detect increased local pressure caused by both malignant and benign breast lesions, and that a pressure threshold for malignancy could be established," the authors wrote. And that's precisely what happened.
What they found
The study included 155 women recalled from the Swedish national breast screening program at Skåne University Hospital in Malmö, and the researchers acquired mechanical imaging readings of the symptomatic breast. They defined the relative mean pressure on the suspicious area and established a threshold for malignancy by correlation of local pressure with pathology.
The effect of adding adjunct mechanical imaging to screening was estimated in terms of reduced recall rates, assuming that the radiologist would recommend recall based on the screening mammogram and mark the location of the suspicious finding. The researchers assumed an actual recall would be made only if the local pressure on that feature exceeded the threshold for malignancy.
Of the 155 women, 71 had biopsies -- 50 were benign and labeled biopsy-proven benign. The remaining 84 cases did not warrant a biopsy and were thus very likely, but not certainly, benign. The researchers labeled theses as other benign.
The conclusive cases consisted of the following:
- 11 invasive ductal carcinoma, invasive lobular carcinoma, or tubular
- 2 ductal carcinoma in situ (DCIS)
- 1 non-Hodgkin's lymphoma
- 43 biopsy-proven benign
- 53 other benign
The remaining 45 cases were inconclusive.
Biopsy-proven invasive cancers had a median relative mean pressure on the suspicious area of 3.0, significantly different from biopsy-proven benign at 1.3. Nonbiopsied cases had a median relative mean pressure on the suspicious area of 1.0. The lowest relative mean pressure on the suspicious area for invasive cancer was 1.4 when excluding for DCIS and non-Hodgkin's lymphoma.
With the higher limit, 56 benign cases were below this score, 23 of which were biopsied. In the original population of 155 women, of which 71 were biopsied, this would be equivalent to a reduction of recall rates by 12% and 36%, respectively, with the biopsy rates likewise decreasing by 13% and 32%, respectively, according to the authors.
"The results suggest a definable lower [relative mean pressure on the suspicious area] threshold for malignant breast cancer, below which all suspicious findings were benign," they wrote. "This is consistent with our hypothesis and earlier results in the field."
The results are all the more surprising considering all the technical issues the team experienced using its improvised setup, Dustler noted.
"Despite the various problems, the size of the results (the potential reduction of recalls and biopsies) was larger than we had expected," he pointed out. "If the results hold and a similar pressure sensor system can be integrated into screening practice, reducing recalls by more than a third would help reduce the workload of radiologists and allow them to focus more on the truly suspicious cases, basically providing information similar to that normally requiring an ultrasound examination already during the screening step."
Dustler and colleagues are currently in the process of starting a much larger follow-up study to confirm the results.