The European Society of Urogenital Radiology (ESUR) has updated its guidance on MRI of the sonographically indeterminate adnexal mass integrating functional techniques. One of the more significant changes concerns solid adnexal masses with low T2 signal, for which diffusion-weighted imaging (DWI) is recommended now.
ESUR previous guidelines from 2010 suggested a basic examination involving T1- and T2-weighted imaging to determine the nature and key signal characteristics of the mass, supplemented by additional oblique T2-weighted imaging, fat-suppressed T1-weighted imaging, or contrast-enhanced T1-weighted imaging, depending on the key characteristic of the mass.
"Recently, much effort has been invested in improving presurgical diagnosis of adnexal tumors by developing risk models and scoring systems using sonography," noted the authors, led by Dr. Rosemarie Forstner from the department of radiology at Paracelsus Medical University in Salzburg, Austria, in an article posted online on 21 October by European Radiology.
Indeterminate masses
In clinical routine, 5% to 25% of adnexal lesions will remain indeterminate after sonography and even using the International Ovarian Tumor Analysis (IOTA) group simple rules, 22% of lesions will remain indeterminate on ultrasound. Most turn out to be common benign entities, such as hemorrhagic lesions, fat-poor mature teratomas, uterine leiomyomas, and ovarian fibromas.
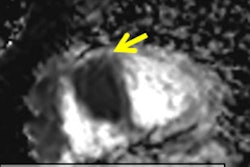
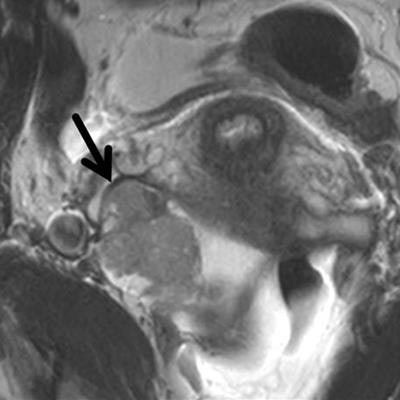
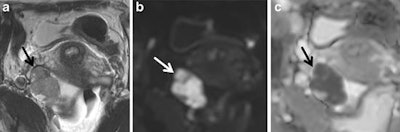 Ovarian carcinoma confined to the right ovary (arrow) displaying intermediate signal intensity on T2-weighted imaging and restricted diffusion characterized by high signal intensity on the high b-value (b = 1,200) image and loss of signal on apparent diffusion coefficient. All images courtesy of Dr. Rosemarie Forstner.
Ovarian carcinoma confined to the right ovary (arrow) displaying intermediate signal intensity on T2-weighted imaging and restricted diffusion characterized by high signal intensity on the high b-value (b = 1,200) image and loss of signal on apparent diffusion coefficient. All images courtesy of Dr. Rosemarie Forstner."The clinical impact of defining whether an indeterminate mass is benign or malignant is enormous," they wrote. "Women believed to have ovarian cancer may require radical cytoreductive surgery by a specialist surgeon in gynecological oncology. Furthermore, women with suspected malignancy may require transfer to a specialist institution. Conversely, benign adnexal masses may either be managed conservatively or undergo simple resection by a general gynecologist."
This makes identifying these masses all the more important. In their original guidelines, Forstner and colleagues suggested where radiologist supervision of the examination was possible, an algorithmic approach could be used to tailor the examination, and, in most cases, an accurate diagnosis could be achieved using one or two "problem-solving" sequences in addition to the compulsory sequences.
The updated MR imaging protocol is as follows:
| Updated MR imaging protocol on adnexal masses | |
| Patient preparation |
|
| Basic MR sequences |
|
| Problem-solving sequences |
|
Other recommendations include no change in the evaluation of T1 "bright" masses -- their fat or blood content can be determined using a combination of T1-, T2-, and fat-suppressed T1-weighted imaging.
"When there is concern for a solid nodule within such a mass, it requires additional assessment as for a complex cystic or cystic-solid mass," the researchers wrote.
They now recommend DWI be applied for solid adnexal masses with low T2 signal because such masses with low DWI signal can be regarded as benign. However, any solid adnexal mass that shows intermediate or high DWI signal requires further assessment by contrast-enhanced T1-weighted imaging, ideally with dynamic contrast-enhanced MRI, they added.
"This technique may also be useful in the differentiation of uterine from ovarian origin in such a mass," they added.
Forstner and colleagues also now recommend that both DWI and dynamic contrast-enhanced MRI be used, if available, for complex cystic or cystic-solid masses; otherwise, such masses are appropriately examined using contrast-enhanced T1-weighted imaging.
The authors also had specific updates on the imaging technologies.
DWI
Several studies have confirmed DWI has a valuable role in MR imaging of the adnexal mass, but the correct DWI technique is ensured by using a high enough b-value to suppress any high signal intensity from freely diffusing water molecules, while keeping sufficient signal-to-noise ratio to identify pathology that has restricted water diffusion, the authors noted.
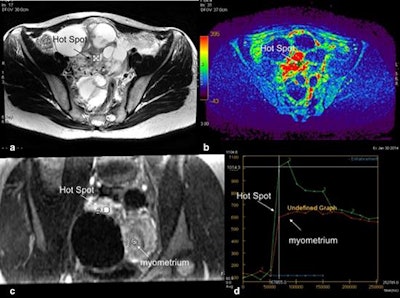 Technical assessment of dynamic contrast-enhanced MR imaging in complex adnexal masses. This example shows a complex right ovarian mass with a solid component in intermediate T2-weighted signal (a) that heterogeneously enhances after gadolinium injection. Parametric map (maximal slope) helps to determine the most suspicious location (hot spot) where the region of interest should be placed to build the time-intensity curve (b). To compare this curve with the myometrial curve, 3D T1-weighted sequence must be reformatted in the coronal plane to place the two regions of interest (solid component and external myometrium) (c). Comparison of time-intensity curves shows the solid component enhances according to a time-intensity curve type 3 (curve steeper than that of myometrium).
Technical assessment of dynamic contrast-enhanced MR imaging in complex adnexal masses. This example shows a complex right ovarian mass with a solid component in intermediate T2-weighted signal (a) that heterogeneously enhances after gadolinium injection. Parametric map (maximal slope) helps to determine the most suspicious location (hot spot) where the region of interest should be placed to build the time-intensity curve (b). To compare this curve with the myometrial curve, 3D T1-weighted sequence must be reformatted in the coronal plane to place the two regions of interest (solid component and external myometrium) (c). Comparison of time-intensity curves shows the solid component enhances according to a time-intensity curve type 3 (curve steeper than that of myometrium).For the female pelvis, use the urine in the bladder as an internal reference to guarantee the chosen high b-value is satisfactory. The urine is high in signal intensity at b0 and decreases as the b-value increases. When the bladder signal intensity is fully suppressed, the optimal b-value for adnexal mass characterization is achieved, they added.
For gynecological imaging characterization, the optimal b-value is usually 800 s/mm2 to 1,000 s/mm2, but it may be increased up to 1,200 s/mm2 or 1,400 s/mm2.
The key points for the interpretation of DWI are as follows:
- DWI signal intensity of water (i.e., urine in the bladder) is dark.
- The DWI signal intensity of the mass must be compared with that on T2-weighted imaging and apparent diffusion coefficient (ADC).
- Due to considerable overlap, ADC quantification is not useful for assessing adnexal masses. There is no indication to perform multiple b-value diffusion.
DWI should not be used to diagnose mature ovarian teratomas and endometriomas; the great majority of these lesions can be accurately diagnosed by observing their T2-weighted features and the characteristics on T1-weighted imaging and fat-suppressed T1-weighted imaging.
"The added value of DWI is in assessing nonfatty, nonhemorrhagic pelvic masses that are entirely solid or complex masses that are either septate cysts or complex solid and cystic masses," the authors noted.
DWI increases diagnostic confidence by about 15% when added to conventional images, they added.
An MRI scoring system based on standard T1- and T2-weighted imaging appearances supplemented by DWI and dynamic contrast-enhanced MRI features (ADNEX MR scoring system) has been proposed, and a prospective multicenter study is being conducted.
The prospective study is being done in tandem with the female pelvic imaging working group of the ESUR (EURAD-MR Classification) to analyze the potential impact of this model on therapeutic strategy and test its reproducibility, Forstner and colleagues wrote. The first results are expected this year.