As treatment options for adnexal masses get more sophisticated and patient-specific, determining the location, size, and likelihood of malignancy of a lesion are becoming increasingly important, Portuguese researchers have underlined.
"A systematic, step-wise approach to imaging analysis, associated with the knowledge of MRI specific findings in ovarian cancer, is fundamental for identifying the multiple ovarian cancer mimics," noted Dr. Eva Baptista, from the department of radiology at Hospital Curry Cabral in Lisbon. "Subdividing ovarian cancer mimics into groups according to their morphologic features helps, narrowing down the differential diagnosis."
Ovarian cancer accounts for 4% of cancers in women and is responsible for 5% of cancer deaths, so predicting the likelihood of malignancy in a patient who presents with an adnexal lesion is of the utmost importance, she told delegates at the recent European Society for Magnetic Resonance in Medicine and Biology (ESMRMB) congress in Lisbon. Such predictions directly affect the surgical decision, including the therapeutic approach and surgical technique.
Because endoscopic surgery is becoming ever more popular, pretreatment imaging evaluation should diminish the possibility of encountering an unexpected ovarian cancer, and even the need for subspecialty cooperation, she explained.
"Thorough pretreatment assessment by cross-sectional imaging plays a pivotal role in the management of a suspected adnexal mass, but despite well-established imaging criteria for ovarian cancer, findings in malignant and benign lesions overlap and a variety of ovarian cancer mimics contribute to the complexity of imaging interpretation," Baptista pointed out.
Using a dedicated protocol and a systematic approach to imaging interpretation, MRI can be a valuable problem solver in the evaluation and differentiation of a suspected adnexal lesion. Her groups uses a 1.5-tesla MR system with a pelvic phased-array coil and the following protocol: T2 fast spin echo (FSE) axial (5mm/0.5mm), T2 FSE sagittal (4 mm/0.4 mm), T1 FSE in the axial plan of the ovary (4 mm/0.4 mm), T2 FSE in the axial plan of the ovary (4 mm/0.4 mm), T1 in the axial plan of the ovary, with fat suppression or T1 axial 3D with fat suppression and IV contrast (dynamic study), (4 mm/0.4 mm).
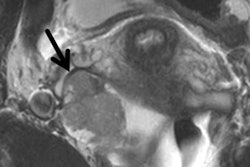
Defining the origin of a pelvic mass requires a practical approach, according to Baptista. The presence of adjacent ovarian follicles indicates an adnexal lesion, as does the so-called beak sign (a mass deforming the ovary into a beak shape), the ovarian pedicle sign (identifying the ipsilateral ovarian vascular pedicle, leading to the lesion), and the lateral displacement of the iliac vessels.
Conversely, separate identification of the ipsilateral ovary indicates a nonadnexal lesion. The "claw sign" (an embedded lesion, typical in subserosal uterine leiomyoma), along with "vascular bridging vessels sign" (presence of bridging vessels in the interface between the uterus and uterine lesions, usually seen in subserosal leiomyoma), also indicate a nonadnexal lesion, as does "ball on a string sign" (typically encountered in neurofibroma) and medial displacement of the iliac vessels.
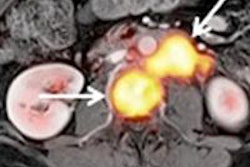
MRI has an accuracy rate of 91% to 95% for differentiating benign from malignant adnexal tumors, she noted. Typical primary findings in ovarian cancer include a size greater than 4 cm, thickness of wall and septa greater than 3 mm, solid or mixed architecture, papillary projections, necrosis and hemorrhage, and contrast enhancement. Ancillary findings are infiltration of pelvic organs or sidewall, peritoneal implants, ascites, and adenopathy.
"Since it is common to find advanced disease at initial presentation (FIGO III and IV), ancillary findings increase the diagnostic confidence for ovarian cancer," Baptisa stated, adding that in her group's series, they encountered no cases of adnexal mature solid teratoma, isolated Brenner tumor, and MRI of an ovarian hyperstimulation syndrome.