The management of breast lesions with uncertain malignant potential (B3 lesions) will take center stage at the annual scientific meeting of the European Society of Breast Imaging (EUSOBI), which begins today in Paris, and breast imaging pioneer Dr. Christiane Kuhl will focus on MRI's impact on these questionable findings.
"Over recent years, the allegedly limited specificity of breast MRI has been refuted by data, which confirm that the positive predictive value of MRI is as high as that of mammography," said Kuhl, a professor of radiology and the director of the Clinic for Diagnostic and Interventional Radiology at the University of Aachen in Germany. "Moreover, even though MRI and mammography can cause 'false-positive' diagnoses, we found the prognostic implications of false-positive diagnoses in mammography and MRI may not be equivalent."
 A "false-positive" diagnosis in breast MRI can warn of future breast cancer development, Dr. Christiane Kuhl said.
A "false-positive" diagnosis in breast MRI can warn of future breast cancer development, Dr. Christiane Kuhl said.While tissue changes that cause false-positive diagnoses in mammographic screening mainly represent regressive or simple fibrocystic changes, tissue changes that cause false-positive diagnoses in MRI tend to represent proliferative, and frequently even atypical, changes, she explained in an interview before the Paris meeting. As a result, the implications of false-positive diagnoses in MRI and mammography differ: In a woman at average risk undergoing screening, diagnosis of atypical tissue changes will change her future management.
"These women carry a greatly increased risk of subsequent breast cancer and should at least undergo intensified surveillance. Therefore, calling such findings 'false positive' is somewhat misleading," she noted.
Kuhl said genomic changes during breast cancer progression should be reflected in definitions that distinguish "actionable" from "nonactionable" disease, and instead of false positives, specialists should consider using more suitable terms such as "at risk" findings.
"One should keep in mind that medicine needs to dichotomize a biological continuum. Currently, anything up to ductal carcinoma in situ (DCIS) is considered benign, anything after it is considered cancer," she stated. "Atypical ductal hyperplasia (ADH), for example, shares histological features of low-grade DCIS, and these lesions are associated with a similar lifetime risk. However, for DCIS, treatment is administered while ADH is not usually treated at all."
The gap between diagnostic and treatment tools may have some impact on perception, and with more refined and gentle treatments that help prevent the progression to breast cancer in women diagnosed with ADH, such findings will be considered desirable and not labeled false-positive diagnoses, according to Kuhl.
Randomization: Not always the holy grail
At a session today (Friday), "Is there enough evidence for breast MRI?" Kuhl plans to ask delegates what level of proof is sufficient and to urge them to use the terminology of evidence-based medicine carefully.
"Many ask for 'randomized trials' as if this was the holy grail of evidence, yet evidence-based medicine distinguishes between studies that evaluate new treatment methods, and those evaluating new diagnostic tests," she explained.
In drug trials, an intraindividual comparison is unattainable because it is impossible to treat the same patient twice, with two different medications, to see which one works better. Therefore, to evaluate new drugs, patients need to be randomly streamed to the new or established treatment path. Randomization is only a surrogate in situations where intraindividual comparisons are impossible. Conversely, to evaluate the utility of diagnostic tests, it is possible to investigate the same patient twice with two different imaging methods, and to compare the respective accuracy.
"For diagnostic tests, randomization is neither needed nor useful," she stressed.
Kuhl suspects that asking for randomized trials to evaluate preoperative breast MRI is asking for inappropriate evidence. Furthermore, due to differences in surgical styles, the reoperation rate between surgeons of the same institution has been shown to range between 0% and 70%, and she thinks it would be impossible, given this huge variability, for the effects of an improved diagnostic test to shine through in any outcome studies.
"If breast conservation is an aim, knowing the true local extent of a cancer is the single most important prerequisite for successful surgery," she continued. "The Oxford Institute of Evidence-Based Medicine encourages doctors to use the most accurate diagnostic test once its superior accuracy has been proven by intraindividual comparative studies. And this is where we stand with breast MRI. We do not have to wait for evidence from randomized trials; in all likelihood, such evidence will never be available."
Dense breasts
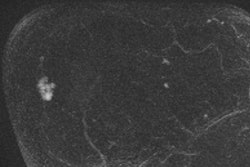
Another hot topic at the EUSOBI meeting promises to be the role of MRI in screening women with dense breasts, following the start of the ECOG/ACRIN (Eastern Cooperative Oncology Group and the American College of Radiology Imaging Network) abbreviated breast MRI screening trial (EA1141) activated earlier this month.
Kuhl, who is the co-principal investigator of this trial, hopes it will change the landscape of breast cancer screening and increase women's access to breast MRI. To date, the only tried and proven screening method for decreasing mortality from breast cancer is mammography, but mammography can miss biologically aggressive cancers, especially in women with dense breast tissue, while picking up indolent slow-growing disease, she explained.

"Mammography detects many breast cancers by depicting regressive changes such as calcifications and architectural distortions, namely hallmarks of pathophysiological changes that reflect slowed growth and cell death. This leads to an effect known as the 'length-time bias.' Overdiagnosis is nothing but an extreme form of length-time bias," Kuhl said.
Conversely, breast MRI is associated with what could be called a 'reverse-length-time bias,' and it works by depicting angiogenic and protease activity, the pathophysiological processes of DCIS and cancers that are closely associated with carcinogenesis and metastatic progression, she explained. "The more aggressive a cancer is, the better seen it is on MRI," she noted.
Overdiagnosis is only one side of the problem, according to Kuhl. The other is underdiagnosis: the failure to pick up cancers that require treatment. Despite decades of mammographic screening, breast cancer continues to represent a major cause of cancer in women, suggesting a need for improved screening strategies.
"Screening is not about finding all cancers and their precursors as soon as possible. Rather, the goal is to find early those cancers that have the potential to kill. Screening tests need to have a sensitivity profile that highlights rapidly growing cancer while downplaying biologically unimportant disease such as low-grade DCIS. And that's exactly what MRI offers," she said.
Kuhl pointed to other advantages of abbreviated MRI (AB-MRI) that included fast acquisition time of three minutes and an image interpretation time of only a couple of seconds to rule cancer out. Such speed would make using it on a broad scale for screening purposes highly feasible. However, she warned it would be difficult to change screening methods because of entrenched habits that tend toward modifying mammography rather than introducing different modalities.
"Based on over 20 years of experience, I'm skeptical that breast MRI will be accepted quickly even though mammography is less accurate, has a less-advantageous sensitivity profile, takes longer to acquire and to read than AB-MRI, and involves breast compression and ionizing radiation," she added.
Much would depend on how willing vendors would be to manufacture MR systems optimized for breast imaging, geared up for the high throughput that screening would require. Currently considered an expensive tool, scanners for AB-MRI breast imaging would also have to carry a lower price tag for use in future nationwide screening programs, Kuhl said.