A new investigational technique is enabling German researchers to perform MR-guided liver biopsies of lesions that can't be seen using other modalities and are inaccessible in most MRI scanners, according to a new study in the August edition of European Radiology.
The researchers from Leipzig University Hospital used an add-on MR navigation system with optical instrument tracking for image guidance and insertion of biopsy devices from outside the magnet bore. A fast control imaging technique allowed them to visualize the true needle position at any time, Dr. Michael Moche and colleagues wrote. The image-guided liver biopsies were performed successfully in 54 patients, with 88% sensitivity and 100% specificity, they noted.
"Using this navigation device, biopsies of poorly visible and difficult accessible liver lesions could be performed safely and reliably in a closed-bore MRI scanner," the study authors wrote (European Radiology, August 2016, Vol. 26:8, pp. 2462-2470).
MRI better when feasible
MRI often does a better job of visualizing small liver lesions than CT or MRI, and its excellent soft-tissue contrast, lack of radiation exposure, and long-lasting contrast media offer advantages as an alternative imaging modality, wrote Moche and colleagues Suzann Heinig, Nikita Garnof, Jolen Fuchs, and Tim Ole-Peterson. Still, the specificity of liver lesions at MRI isn't usually high enough to preclude biopsy.
However, the introduction of image-guided percutaneous biopsy into clinical practice has been a latecomer to the party, because only the newer, open MRI systems offer reasonable access to the patient compared with conventional closed-bore scanners. And even so, open MRI scanners are more expensive to buy and maintain, with lower image quality than closed-bore scanners due to inferior field homogeneity, the authors wrote.
The challenge for the investigators, then, was to find a way to perform liver biopsy in a closed-bore scanner, other than a time-consuming method that involved rough visual estimation of the access point and orientation, but without true image guidance.
"An easy-to-use navigation system allowing fast and accurate determination of the skin entry point and targeting of the lesion in one step outside the bore, would simplify the approach," they wrote. "We report our clinical experience with liver biopsies using an add-on navigation device for a closed-bore 1.5-tesla MRI scanner and evaluate the system's functionality, effect on workflow, and diagnostic accuracy."

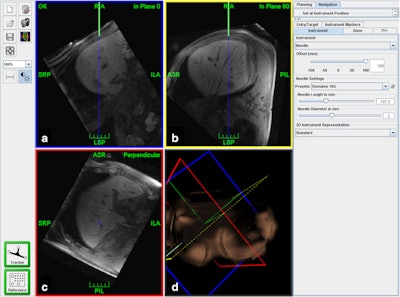
Screenshot of the navigation scene. Reformatted MR images of the planning dataset are interactively shown either instrument-related inplane (a), 90° in-plane (b) or perpendicular to the instrument (c). On a and b, the green lines indicate the needle in full length and the blue lines show its trajectory to facilitate orientation to the target (arrow head). For better orientation, a 3D reconstruction is also provided (d).
The team performed biopsies in 52 patients, including 30 men and 22 women with a mean age of 57.2 ± 13.8 years, and a mean body mass index (BMI) of 26.6 ± 5. The investigators used an add-on MR navigation system (iMRI Navigator, Localite) with optical instrument tracking for image guidance and biopsy device insertion from outside the bore. Using the system, fast control imaging allows visualization of the true needle position at any time.
The patients were scheduled for MRI-guided biopsies based on significantly improved visibility of the suspect lesion on MR images (n = 23) compared with CT and ultrasound, difficult double oblique access path (n = 39), or patient age under 50 years (n = 17). Biopsy workflow and procedure duration were recorded. Histological analysis and clinical course/outcome were used to calculate sensitivity, specificity, and diagnostic accuracy.
Forty of the 52 interventions were performed by an interventional radiologist with 10 years of experience. Two residents performed the remaining exams using a dedicated navigation system with optical tracking and automatic patient registration based on MRI-marker localization. The navigation system allowed the skin entry point to be determined accurately, and allowed for the lesion to be targeted from just one step away from the bore, the group wrote. All biopsies were performed with the patient in a comfortable supine position.
For improved diagnostic image quality, two 19-inch loop coils (Siemens Healthineers) were placed on the patients' abdomen and right side, and used in combination with the spine coil. All interventions were performed in a closed-bore 1.5-tesla MR scanner (Magnetom Symphony, Siemens Healthineers). Marker localization was achieved with a short scan sequence using a low flip angle and large field-of-view (FOV) in three standard views.
For procedure planning, the team acquired transverse images with volume-interpolated breath-hold examination (VIBE), half-fast imaging with steady precession (TRUFI) using the combination of loop and spine coils 15 minutes after administration 10 mL of gadoxetat disodium contrast (Primovist, Bayer HealthCare Pharmaceuticals). During imaging, the operators carefully gave the breath-hold instructions on which the patients had been trained. They used the sequence with optimum visualization for the analysis.
In all, 54 of 55 attempted liver biopsies were completed successfully. One intervention was technically unsuccessful, with the procedure subsequently performed manually. There were no major and four minor complications, the team wrote. One narrow perihepatic and one subcutaneous hematoma were detected on final control imaging, but did not progress at ultrasound. Two patients experienced minor abdominal pain, nausea, and vomiting.
The mean tumor size was 23 ± 14 mm and the skin-to-target length ranged from 22 mm to 177 mm. Sensitivity was 88%, specificity was 100%, and diagnostic accuracy was 92%, the team reported. Mean procedure time was 51 ± 12 minutes, with the puncture itself taking about 16 minutes.
"The accuracy, safety, and duration of the procedure were found to be acceptable for clinical routine use," Moche and colleagues wrote. The 92% accuracy is comparable with previous results for MRI-guided interventions as well as the accuracy achieved using ultrasound and CT guidance, they wrote.
"It should be noted, however, that for our study only those patients were selected who could not be biopsied under CT or ultrasound guidance. Thus, it can be assumed that this selection of difficult cases would have led to a lower accuracy when compared with a randomized cohort," they wrote.
Most common MRI scanners have a bore diameter of 60 cm and a gantry length of 140 cm or higher, which limits patient access and renders MR fluoroscopy (MRF) procedures unfeasible. MRF is especially advantageous in uncooperative patients, but image quality in open or wide-bore systems is no better than for CT or ultrasound, necessitating the use of closed-bore scanners.
The low complication rate in this study highlights the safety of MRI-guided biopsies, and no major complications were documented in this study, consistent with only two reports of major complications in other studies.
A limitation of the system is that it is not yet approved for commercial use. Also, the current study lacked a control group on whom interventions were performed manually for comparison. The authors deemed it too risky to perform without image guidance.
An intervention combining brief respiratory training, navigated needle feed with automatic patient registration and immediate control imaging proved successful for liver biopsies, the study team concluded.
"Access to the patient outside the bore features maximum patient comfort and allows interventional radiologists to take samples with high diagnostic accuracy, even for overweight patients," Moche and colleagues wrote.
Add to that relatively short procedure times and flexibility of the system, and it should be relatively easy to incorporate into the clinical workflow, they added.



















