Cone-beam CT (CBCT) can help identify treatment-relevant anatomical changes in patients receiving proton therapy for lung cancer, according to new research from Belgium, the U.K., and the U.S.
An adaptive lung-cancer proton therapy workflow that makes use of on-board CBCT has been developed. In the identification of treatment-relevant anatomical changes in patients between radiation doses, CBCT gave similar clinical indicators to regular CT scans.
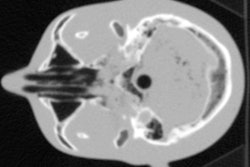
Compared with conventional photon-based radiotherapy, proton therapy allows for greater levels of dose localization, with virtually no exit dose that would result in tissue damage. The procedure comes, however, with certain drawbacks. Patient motion, particularly with pencil-beam scanning, presents one such challenge. Another difficulty lies in proton therapy's higher sensitivity to anatomical changes -- for example, in the lung -- that can affect the distribution of the radiation dose.
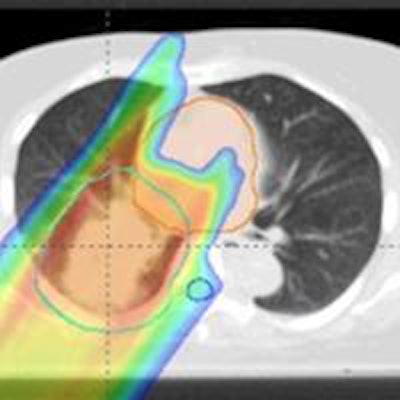
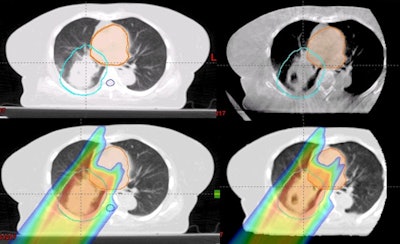 Top row (left to right): The planning CT and CBCT. Bottom row: The dose distribution on the planning CT, and on the virtual CT generated from the CBCT. Images courtesy of Boon-Keng Teo, PhD.
Top row (left to right): The planning CT and CBCT. Bottom row: The dose distribution on the planning CT, and on the virtual CT generated from the CBCT. Images courtesy of Boon-Keng Teo, PhD.Tumor enlargement or lung collapse, for example, can result in a shortened beam penetration, reducing coverage of the target. In contrast, tumor shrinkage can result in the radiation beam penetrating further than intended, damaging regular tissues. To compensate for this, regular CT scans are taken during the course of treatment to identify anatomical changes and adjust the therapy accordingly.
One alternative to these routine CT scans lies in the use of CBCT, which uses divergent x-rays to create a 3D image. CBCT comes with a number of advantages, offering highly accurate patient positioning, as well as the capacity to monitor the patient in the treatment position and to rapidly assess the current treatment dose.
In their new study, Boon-Keng Teo, PhD, a radiation oncologist at the University of Pennsylvania, and colleagues, has developed a CBCT-based workflow for adaptive proton therapy. First, prior to each individual proton treatment, patients are given a CBCT scan. From this, a virtual CT scan is generated by deforming the treatment's original planning CT scan onto the geometry of the current CBCT scan.
An additional correction step accounts for specific anatomical changes -- such as large tumor regressions -- that cannot be handled by the deformable image registration alone (International Journal of Radiation, Oncology, Biology, and Physics, 3 February 2016).
From this, a fast, range-corrected dose distribution of the intended treatment is calculated. If the identified dosimetric changes are found to be within safe limits, treatment may proceed -- else, an offline review of the virtual CT is called for, which may lead to a replan CT to adjust the treatment accordingly.
To test the concept, the researchers compared their CBCT-derived virtual CTs with corresponding, conventional CT scans of 20 lung cancer patients who exhibited a variety of treatment responses including lung collapse or reinflation, and tumor growth, shrinkage, or density variations.
"A virtual CT generated from a CBCT can give similar dosimetric indicators as a regular CT," Teo said. "In most cases, CBCTs can replace evaluation CTs in proton therapy for assessment of anatomical change, and therefore reduce the frequency of the evaluation CT scans during the course of treatment."
"[This is] the first step toward the clinical utilization of CBCT for adaptive proton therapy, which is essential to fully exploit the physical advantages of proton therapy," said Brian Winey, a medical physicist at Harvard Medical School who was not involved in this study. CBCT, he adds, will allow proton therapy centers to reduce the effects of the range uncertainties that result from anatomical variations during patient treatment.
"Adaptive [proton therapy] workflows based on CBCT and deformable image registration may prove valuable to identify critical cases which may require correction strategies," said Katia Parodi and Guillaume Landry, medical physicists at Ludwig-Maximilians-Universität München who were not involved in this study. They add: "[M]ore research needs to be done to carefully validate deformable image registration accuracy and improve CBCT image quality depending on anatomical location, as well as to identify reliable clinical indicators for proper alerts triggering additional actions during the fractionated treatment course."
With their initial study complete, the researchers are now working to further develop and test their workflow, along with looking to apply the same principle to other possible treatment sites.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.