An international team of researchers has developed a statistical tool that improves the resolution of proton imaging in a single step, without any prior radiographic information. The tool, which has so far been tested in computer simulations, has the potential to boost the accuracy of proton therapy so that less radiation is delivered to healthy tissue during cancer treatment (Physics in Medicine and Biology, 3 November 2016, Vol. 61:23, pp. 8232-8248).
Proton therapy is similar to conventional radiotherapy, but, in principle, has a finite range that spares surrounding healthy tissue. To make the most of that finite range, however, requires high confidence in the position of the dose peak. Proton imaging is thought to be the best way of mapping the insides of a patient in order to locate that dose peak, but it suffers from poor spatial resolution as the protons scatter off various atomic nuclei en route to the detector.
Algorithms already exist to enhance the resolution of proton imaging, but they can only "learn" from a large set of radiographic images taken beforehand. "To acquire all these projections is a long and arduous process that delivers extra dose to the patient," explained Charles-Antoine Collins-Fekete of Laval University in Quebec, Canada. "The innovation of this work is that we maximize the spatial resolution for each projection completely independently."
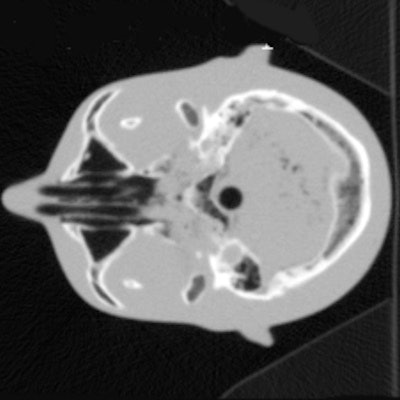
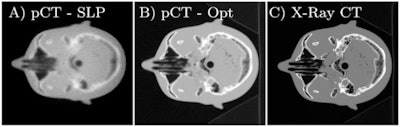 (A) Reconstructed proton CT of a head phantom from the original proton radiography; (B) the reconstruction with the optimized proton radiography; (C) the same slice of the x-ray CT phantom.
(A) Reconstructed proton CT of a head phantom from the original proton radiography; (B) the reconstruction with the optimized proton radiography; (C) the same slice of the x-ray CT phantom.Collins-Fekete and colleagues, who are based at Laval and other institutions in the U.S. and Belgium, developed their tool by exploiting the fact that protons are more likely to scatter through some tissues than others. Once a preliminary map of tissue has been delivered by proton imaging, therefore, it is possible to estimate statistically the likely route the protons must have taken in order to produce it. Then, it is possible to retrieve the image that would have been acquired, had the scattering not taken place. "The idea of using a path estimate to optimize proton radiography independently is a new one," Collins-Fekete said.
In computer simulations, Collins-Fekete and colleagues tested their statistical tool -- which they call a "maximum likelihood least squares estimator" -- on three different tissue phantoms. Adopting a widely used metric for the quantification of spatial resolution in imagery, known as MTF10%, the researchers found they could improve the resolution of a bare proton image with their tool by 65%. The resolution boost was the same as that delivered by existing methods, even though it required no prior radiographic imagery.
"The real advantage is that you can acquire a single [radiographic image] and improve it independently, which was impossible earlier," Collins-Fekete said. "That means proton radiography can directly be used for many applications, such as accurate positioning of the patient before the treatment and monitoring the patient's potential physiology change."
Although the tests currently reported were computer simulations, the researchers already have preliminary results from real detectors. "The first results follow closely our prediction," Collins-Fekete said. "This makes us quite confident that the technique could be brought to a clinical environment without too much delay."
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.